Leveraging CME Requirements to Improve Palliative Care Delivery

It is a hard truth that inadequate clinician training, leading to inappropriate prescribing, was one of several underlying causes of the opioid epidemic. As policymakers and health officials revisit policy interventions to address this crisis, many states have taken action to hold health care professionals (particularly prescribers) more accountable for safe and effective pain management – including establishing new topic-specific continuing medical education (CME) requirements. Given the overlap between many of these new requirements and palliative care knowledge and skills, the Center to Advance Palliative Care (CAPC) conducted three national scans in 2017, 2019, and 2022 to better understand the CME landscape, and identify new or expanded opportunities for palliative care education.
Benefits and Drawbacks to CME Requirements
Continuing Medical Education (CME) requirements can be a powerful tool to ensure that all physicians (MDs and DOs) remain up to date on the state of medical science, as well as new evidence-based interventions. Continuing education (CE) is an expectation across most professions, both in and out of health care. These requirements are an acknowledgement that professions are always changing – old techniques and understandings are refined or discarded, while new ones emerge – and that it is professionals’ responsibility to stay up-to-date after they have completed their initial training. Recognizing the potential impact of CE requirements, CAPC and the National Palliative Care Research Center’s (NPCRC) 2019 State-by-State Palliative Care Report Card included a recommendation for states to explore the feasibility of revising “state health professional licensure and continuing education requirements to include a minimum number of hours of instruction in both communication skills and symptom management skills.”
CME requirements can be a powerful tool to ensure that all physicians remain up to date on the state of medical science, as well as new evidence-based interventions.
Yet while most state licensing boards which govern health professions require a minimum number of approved CE hours (these requirements vary by state and discipline), the landscape of topic-specific CE requirements is more complex. Turning back to CMEs specifically, many states are reluctant to “micromanage” physician education. One reason is respect for professional autonomy and expertise – the majority of physicians know better than legislators or regulators about which topics will enhance their practice. This is especially true given the heterogeneity of physician specialties and key competencies that each are expected to master. Another reason is the number of “important” topics; there is no limit to the number of worthwhile areas in which physicians should seek additional training, ranging from care of patients with specific diagnoses to emerging therapies and interventions. To mandate all would be infeasible, and navigating such requirements would be unmanageable for physicians.
What We Found
Note: CAPC’s most recent scan on CME requirements was conducted in 2022. Please visit CAPC’s resource “Locating Discipline-Specific Palliative Care CE Requirements by State,” which includes the Federation of State Medical Boards’ up-to-date listing of national CME requirements, as well as aggregators for Nurse and Social Work continuing education requirements.
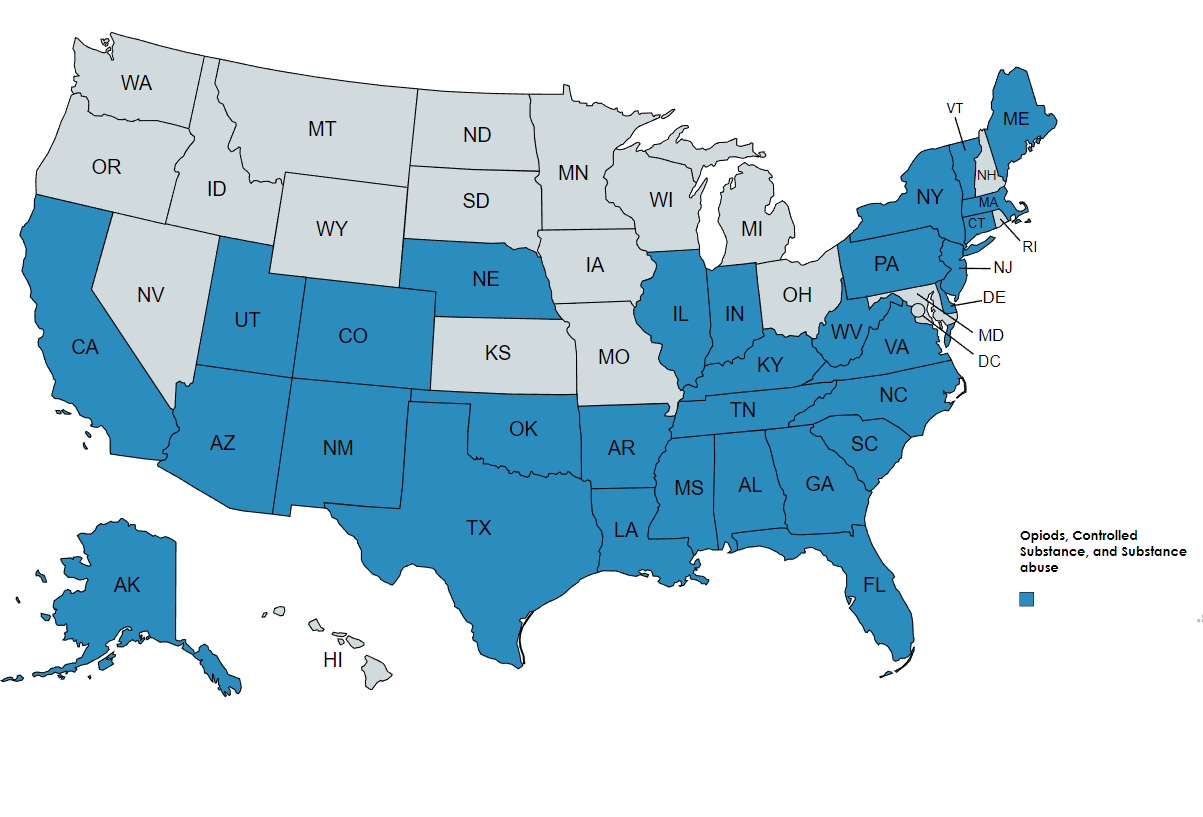
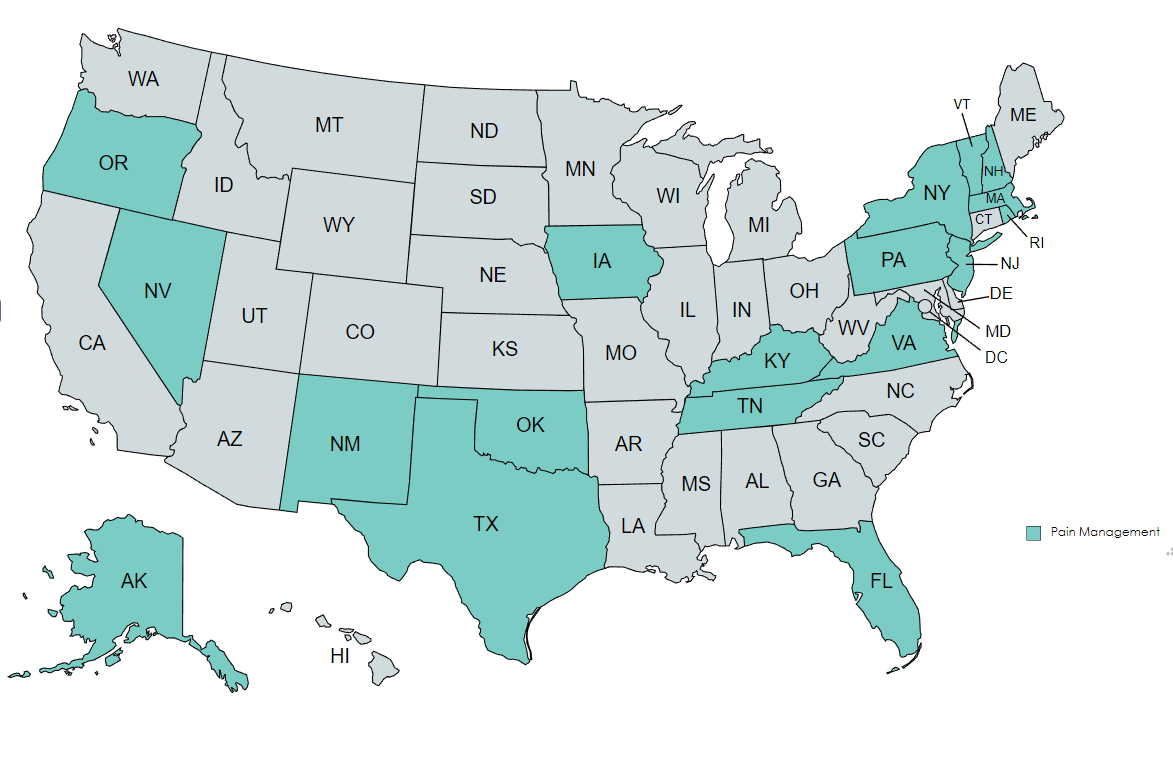
That said, CAPC’s scan and related research on state CME requirements highlighted an important exception – namely that officials will establish physician requirements in response to a public health crisis. We observed the proliferation of requirements related to opioid prescribing (in 32 states) and/or pain management (in 20 states) over the last several years. We also learned that there was a similar wave of state CME requirements related to HIV/AIDs in the late 1990s/early 2000s. We were struck by a few similarities between these two instances, both of which led to new and wide-ranging CME requirements:
- Physician leadership was needed to address these epidemics by delivering care in accordance with evidence-based guidelines; this included assessing for risky behaviors, safely and effectively prescribing, educating patients, and reducing stigma.
- Most physicians received inadequate training during their initial medical education on how to respond to these topics.
- The evidence base supporting how to best respond to these crises continued to evolve rapidly after physicians received initial guidance, justifying the need for ongoing training requirements.
Even with compelling reasons for establishing topic-specific requirements, however, we also observed that there was (and will likely continue to be) churn. For instance, only a few states have retained HIV/AIDS-specific requirements to this day. And Maryland was the first state to abolish its opioid prescribing CME requirement due to a law that prohibited the Board of Physicians from requiring any specific topics as a condition of license renewal. Therefore, while we anticipate that opioid prescribing CME requirements will remain prevalent for several years to come, these might decline as the crisis evolves.
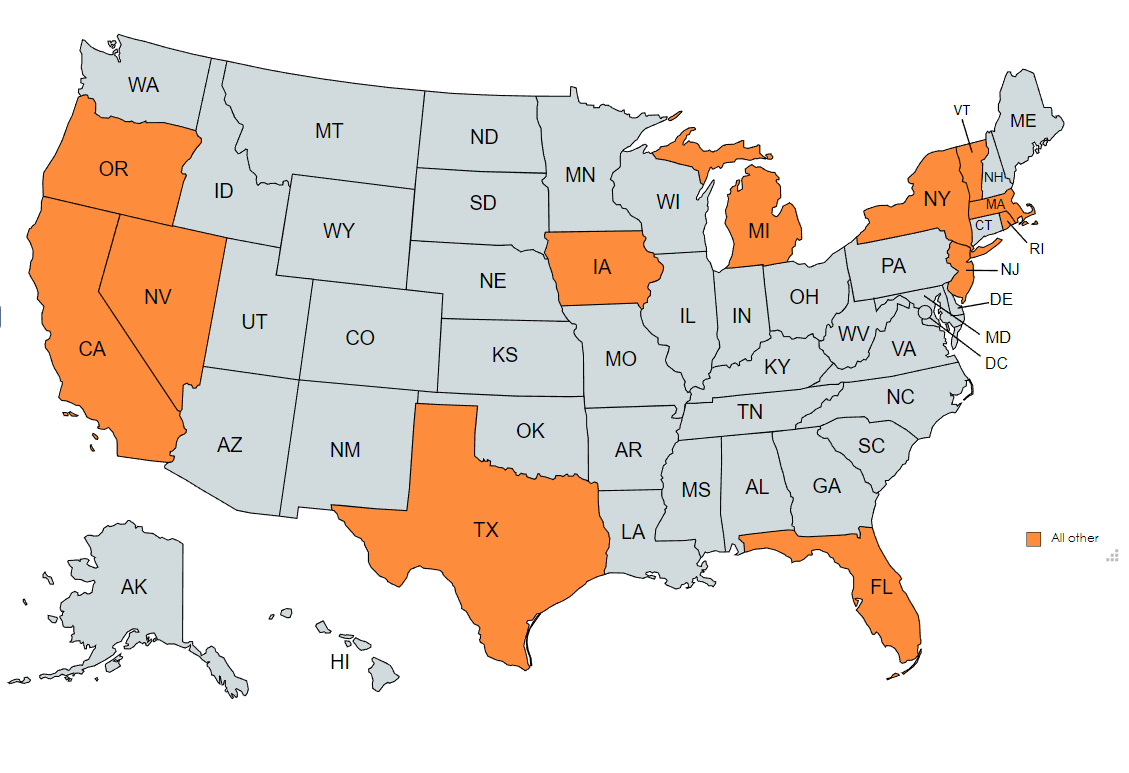
Beyond opioid prescribing and pain management, most states have relatively few topic-specific CME requirements. Among these, however, are many that are relevant to palliative care, including end-of-life care, geriatrics, Alzheimer’s disease, and ethics. And three states (New York, Rhode Island, and Vermont) specifically reference palliative care as part of their CME requirements. The drawbacks are that these requirements count for a relatively small portion of overall required hours, and most are referenced as part of a menu of options rather than true requirements. Interviewees in some states also noted that quality control for some of these “lower profile” requirements is limited (e.g., as long as the topic is mentioned in a course, it counted as meeting the requirement).
The Continued Utility of Topic-Specific CME Requirements
Despite the drawbacks, topic-specific CME requirements present an opportunity to improve the capacity of all physicians to deliver high-quality care to people living with serious illness and their families. Much of what we know about the care of this population reflects the circumstances that led CME requirements in opioid prescribing and HIV/AIDS care – namely that physicians play a critical role in care, but most have not received any formal training in how to: 1) initiate meaningful communication with patients about what matters most to them, and 2) effectively manage complex pain and other symptoms that often accompany serious illness. As more people live longer with serious and complex illness, this gap in preparation contributes to unnecessary suffering, crisis hospitalization, and preventable spending.
Despite the drawbacks, topic-specific CME requirements present an opportunity to improve the capacity of all physicians to deliver high-quality care to people living with serious illness and their families.
Therefore, we encourage palliative care champions to prioritize “Clinician Skill Building” as a state-level goal via exploring the feasibility of establishing CME requirements in communication and symptom management. Consider the following:
- Frame the need for physician continuing education in the context of the public health crisis that it is; The Case for Improving Communication and Symptom Management Skills includes evidence to support this.
- Anticipate resistance to establishing these requirements; understand the reasons for this resistance and proactively collaborate with stakeholders (especially the state medical associations and licensing boards) to develop a mutually acceptable path forward. Strategies could include joining these associations, participating on relevant workgroups, and setting meetings with staff.
- When possible, make communication and/or symptom management a required topic, rather than part of a menu.
- Develop clear subregulatory guidance about what must be covered on each of the topics in order to “count” as meeting the CME requirement.
How CAPC Can Help Physicians Meet State CME Requirements
In the meantime, existing state CME requirements provide an opportunity to advance palliative care knowledge. Increased physician training in communication skills, as well as pain and symptom management, can lead to improved patient experience, safer practices, reduced hospital days and patient spending, less staff burnout, and reduced unnecessary ED and hospital utilization. CAPC has dozens of online courses that can help all physicians meet palliative care-relevant CME requirements across the country – and many of these courses also provide ABIM MOC (Maintenance of Certification) points, which are free for physicians to take under their organization’s membership. We have listed specific courses per topic-specific state requirements in the section below.
CAPC has dozens of online courses that can help all physicians meet palliative care-relevant CME requirements across the country.
An Overview of State Requirements
The following maps provide a general overview of states with requirements that could apply to MDs, DOs, and/or prescribers. They are for informational purposes only; please contact your relevant state boards directly for more information.
Opioids/Prescribing
CAPC courses that can help meet these state requirements for opioids/prescribing include:
- Chronic Pain Strategies for Patients with Serious Illness (new curriculum)
- Assessing Risk for Opioid Substance Use Disorder
- Opioid Trials: Determining Design, Efficacy, and Safety
- Prescribing an Opioid
- Prescribing Short-Acting Opioids: Four Case Studies
- Monitoring for Opioid Efficacy, Side Effects, and Substance Use Disorder
- Converting from Short-Acting to Long-Acting Opioids
- Prescribing Practice and Opioid Conversions
- Advanced Conversions and Opioid Side Effects
General Pain/Symptom Management*
CAPC courses that can help meet these state requirements for general pain/symptom management include:
- Chronic Pain Strategies for Patients with Serious Illness, full curriculum including comprehensive training in chronic pain management, risk mitigation, assessing opioid misuse, and assisting with access to treatment for opioid use disorder (OUD) for patients living with serious illness. (New!)
- Pain Management, full curriculum of 14 courses covering comprehensive pain assessment, choosing the right treatment modality, safe opioid dosing and monitoring, assessing for risk of opioid use disorder, and managing pain in seriously ill patients with concurrent opioid use disorder.
- Symptom Management, full curriculum including assessment and treatment of common sources of misery including shortness of breath, nausea, depression, and constipation.
* Note that Michigan specifies “pain and symptom management” in their requirements, whereas the other states refer only to pain management, assessment, and/or treatment
Other Related Topics (Palliative Care, Geriatrics, Alzheimer’s, Ethics, End of Life)
CAPC courses that can help meet these state requirements for other related topics include:
- An In-Depth Look at Palliative Care and Its Services
- Communication Skills, full curriculum
- Building Physician Skills in Basic Advance Care Planning, full curriculum
- Best Practices in Dementia Care and Caregiver Support, full curriculum
CAPC’s complete online clinical training curriculum can be found here.

