Take Action: Tips for Leveraging the 2019 State-by-State Report Card and State Reports
This post has been updated to include CAPC's new individual State Reports and additional opportunities for action.
Providing hospital palliative care services to our nation’s seriously ill patients is a critical component of quality health care. Palliative care has been shown, in multiple settings, patient populations, and disease types, to improve patient and family caregiver quality of life, strengthen communication with clinicians about preparation for what to expect, and reduce occurrence of symptom crises resulting in emergency hospitalizations. Hospitals must deliver high-quality care for their most seriously ill and complex patients while remaining financially viable, and palliative care is essential to achieving this goal. However, reliable access to these services will only be possible through concerted efforts to drive supportive public policy, ensure reliable financing, and increase professional and public awareness of palliative care and its benefits.
The 2019 State-by-State Report Card ("Report Card") provides an analysis of whether patients living with a serious illness in the United States have access to hospitals with palliative care programs. The primary goals of the Report Card are to increase awareness and inspire action among key stakeholders, and to provide policy recommendations for state and federal policymakers, as well as the private sector including health systems, accountable care organizations, health plans, and employers.
Additionally, in May 2020, CAPC released new state-level reports that build on the Report Card by describing the availability of hospital palliative care in each state as compared to national and regional measures. These reports also provide information on community palliative care, certified palliative care clinicians, and opportunities for quality improvement.
As a palliative care champion, there are many ways to leverage the Report Card and the complementary individual state reports to improve palliative care access locally and nationally. Follow these three steps to take action, and make lasting change for our nation’s sickest patients:
Step 1: Interpret Your State’s Grade
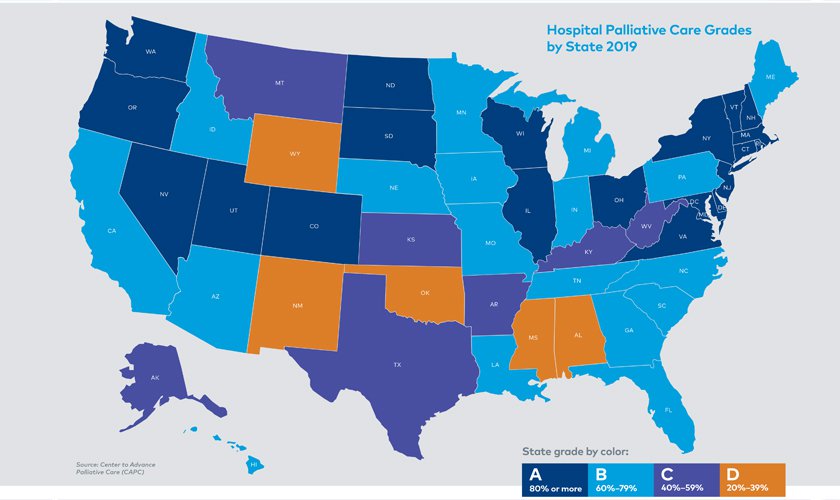
The Report Card calculates the percentage of hospitals with fifty or more beds in a state that have a palliative care program, and assigns a grade based on that percentage. Grades fall into the following ranges: A: 80% or more; B: 60%-79%; C: 40%-59%; D: 20%-39%.
- If your state received an A, your state has a relatively high prevalence of hospital palliative care programs. If a hospital in your state does not offer palliative care, it is lagging behind many of the other hospitals in the state in providing this vital service. However, even in states where more than 80% of hospitals provide some level of palliative care services, variation in staff capacity to meet demand for services, and program characteristics means that not all patients living with a serious illness who would benefit from palliative care have access to it in that state, and there is room for improvement.
- If your state received a B, C, or a D, your state has a relatively low prevalence of hospital-based palliative care programs. This means that a significant percentage of hospitals have not yet established programs, and therefore, many seriously ill patients do not have access to palliative care when admitted. A hospital with an established palliative care program in a B, C, or D state is leading the way to provide high-value care to patients in need and, in some cases, may only be one out of a handful of hospitals to offer this essential service in the surrounding area.
Some additional context can be helpful in interpreting your state’s grade.
For instance, regardless of the grade, specific types of hospitals are more likely to provide palliative care. Hospitals with 300 or more beds, teaching hospitals, non-profit hospitals, and Catholic Church-operated hospitals, all have rates of palliative care above 80%. Hospitals that fall into any of these categories that do not currently offer palliative care are significantly lagging, regardless of where they are located in the United States or their state’s grade.
Step 2: Complete the Story
While the Report Card provides a critical foundation to understanding palliative care access in your state, be aware that these grades do not tell the complete story. Hospitals with fewer than fifty beds are not included in the state grade (see the table on page 38 and the section on “Hospitals with fewer than fifty beds” on page 14 in the Report Card for more information). The Report Card also does not contain information on the quality, staffing, or reach of these hospital palliative care programs. And the Report Card does not include palliative care programs operating in the community, such as those providing services in clinics or office practices, in the home, or in long-term care facilities.
The individual state-level reports provide more details to the story. These details include more granular information on how hospital access in your state compares to access in your region and nationally, and map out where hospital palliative care exists so that you can identify potentially underserved areas. The reports also highlight the number of known community palliative care programs and certified clinicians, as well as the number of organizations in your state that have CAPC membership. All of these data points are intended to provide a more complete picture of your state’s current palliative care capacity to inform future action. These reports do not provide information on quality, staffing, or reach.
Therefore, it is important for palliative care champions to build on the findings of the 2019 State-by-State Report Card and individual state reports by locating as much of this information as you can.
You may have access to more information about palliative care in your state through a State Palliative Care Association (e.g., New York or Minnesota), State Palliative Care Advisory Council, or Comprehensive Cancer Control Program. Some states, such as Florida and California, have conducted research on local access, which contain useful information and could serve as a template for other states. Collecting more information about program availability, reach, and quality will help you identify and priorities opportunities for action. The new Palliative Care Policy GPS is also a useful tool to learn more about policies in your state that may support palliative care, and identify potential areas for policy action.
To help track the growth of palliative care and understand how palliative care programs are meeting national guidelines on programmatic and clinical quality, champions should also encourage all palliative care programs to participate in the Palliative Care Quality Collaborative (PCQC). Launched in 2020, the PCQC is a 501(c)3 organization which houses a new national palliative care data registry. The PCQC Registry collects programmatic data on palliative care operations, staffing, and features. The collaborative combines the National Palliative Care Registry™ (former project of CAPC and the National Palliative Care Research Center), Mapping Community Palliative Care (former project of CAPC and the National Coalition for Hospice and Palliative Care), the Palliative Care Quality Network (PCQN), and the Global Palliative Care Quality Alliance (GPCQA). It provides palliative care programs with reports that compare them to similar programs on structure and process, at no cost. For an additional fee, PCQC will also collect clinical patient-level data to drive quality improvement and reporting.
The findings from PCQC provide users with better snapshots into access, availability, and quality across the continuum of care. And it has also launched its first iteration of program reports. Visit the PCQC website to learn more about this and future opportunities to participate.
Step 3: Establish Goals and Take Action
The Report Card can be a catalyst for conversations about how to ensure that all patients with serious illness have access to high-quality palliative care. The Report Card includes information that is relevant to multiple audiences, ranging from hospital administrators to state health departments to federal legislators. Below are sample activities for how champions can leverage the Report Card to achieve their goals.
Goal: Drive federal support for palliative care
- Incorporate the Report Card into meetings with federal policymakers to frame the need for palliative care access in your state and nationwide.
- Identify palliative care gaps and opportunities; implement relevant recommendations from the Report Card Policy section.
How to Use the Report Card to Support Federal Policy Changes
- Given the large size of the Federal Government and diversity of actors, the Report Card breaks out these policy recommendations into two buckets – Federal Legislation (key audience: Congress) and Federal Regulation (key audiences: Centers for Medicare and Medicaid Services, National Institutes of Health, etc.). For any meeting, make sure that you match any selected policy recommendations to the appropriate audience; otherwise, those you meet with might politely nod their heads and go about their business without taking any action!
- If you meet with your Senators and/or Representative (or more likely their staffers), first take a few moments to ensure they understand what palliative care is. While many will say they know, it is important to have a clear “elevator speech” to avoid potential confusion or misperceptions. There is excellent language starting on page 4 of the Report Card defining palliative care and its positive impact on quality, cost, and patient and family satisfaction. If time allows, share a personal story.
- Second, review your state’s grade (starting on page 8), noting any changes over time. Include high-level details you learned in your “Step 2: Complete the Story” fact-finding – and if you think any progress is linked to specific actions taken by your legislators, thank them! Then note that, despite any progress, there are still patients in need of palliative care who do not have access.
- Finally, select 2-3 top recommendations (starting on page 20) that you want to focus on with your legislator. This can be based on your passion or expertise, but also try to do some homework in advance. Do they sit on a committee that focuses on workforce issues? Then select a recommendation from “Workforce” or “Clinician Skill Building.” Have they spoken in the past about the rising costs of health care or the need for accountability? Then identify a recommendation or two from “Payment” or “Quality, Standards, and Research.” Explain what the recommendation is and how it will help patients with serious illness. Offer to serve as a resource moving forward – subject matter expert, pilot site, speaker. And make sure to thank them for their commitment to improving patient quality of life!
Goal: Increase state recognition and support for palliative care
- Partner with local organizations that focus on improving care for people living with a serious illness to promote Report Card and individual state report dissemination.
- Incorporate the Report Card and your individual state report into meetings with state policymakers (e.g., legislators, State Medicaid Directors) to frame the need for palliative care access in your state.
- Identify state-specific palliative care gaps and opportunities, implement relevant recommendations from the Report Card and individual state report policy sections.
- Incorporate Report Card and individual state report findings into State Palliative Care Advisory Council (or similar body) deliberations, and leverage the findings and policy recommendations to support the agenda.
How to Use the Report Card and State Reports to Support State Policy Changes
State officials, including legislators, department and agency staff, and other state employees, are interested in learning about opportunities to improve quality of life and the value of health care for their residents. When meeting with your representatives or other state leaders to discuss the Report Card and your individual state report, several tips in the Federal section apply; i.e., explain palliative care, tell the story, do your homework to ensure you understand your audience’s priorities. In addition to highlighting your state’s grade, review how your state compares to others in your region – in this case, a little healthy competition can be helpful!
What sets state-level meetings apart is that they provide an excellent opportunity to be specific! When you were “completing the story,” what did you learn about opportunities and barriers in your state? For instance:
- Is there a specific region in which there is concentrated need, and a new or expanded palliative care program could dramatically improve patient access?
- Does your state struggle to hire and retain palliative care specialists?
- Has there ever been a palliative care awareness campaign?
- Does the Palliative Care Policy GPS show innovative policies in other states that you think would be beneficial to replicate?
The Report Card’s state policy recommendations (starting on page 26) are broken out into “Workforce,” “Payment,” “Quality, Standards, and Research,” “Clinician Skill Building,” and “Public and Clinician Awareness”; the individual state report prioritizes these recommendations. Based on your state findings – including your knowledge of what is feasible in the local policy environment – select 2-3 top recommendations that most directly address the highest priority gaps. This section is full of examples of initiatives from other states that you can model your work on.
Goal: Launch or expand a palliative care program in a hospital or local community
- Incorporate the Report Card into meetings with administrators and program funders to provide greater context on the need that your program could fill.
How to Use the Report Card and State Reports with Local Leaders and Funders
Leveraging the Report Card and individual state report with your C-suite, funders, or other key stakeholders will depend on your goals – are you hoping to start a palliative care program? Grow your existing program? Support clinician skill-building? That said, the Report Card can be useful in inspiring action across these audiences because it provides context for your goals. In lower-grade states, the Report Card can create urgency because it highlights large gaps in palliative care access for patients with serious illness. For higher-grade states, there is a great opportunity to cement your reputation as a national leader.
Beyond providing context, it is worth noting that many of the recommendations in the Report Card section, “A Call to Action” (starting on page 16), and those at the end of the individual state reports are not limited to policymakers. Health systems leaders, practices pursuing value, and funders can lend their support to advocacy efforts. There are also many opportunities to go above and beyond by adapting certain recommendations in the “State Policy” section of the Report Card (page 26) and “Purchasers, Health Plans, and Accountable Care Organizations (ACOs)” (page 31) sections. For instance, hospital administrators can review the National Consensus Project (NCP) Clinical Practice Guidelines for Quality Palliative Care and create an organization-wide initiative to bring services into greater alignment with these. Foundations can establish grant programs to support targeted clinical training, helping to advance shared-decision making and quality of life. The benefit of leaders taking independent and early action is that their efforts can help position the state for future success if any policy changes occur; and in the meantime, they are improving care for people who need it the most.
Goal: Educate all clinical staff in communication, pain and symptom management, caregiver support, and when to refer to specialty palliative care
- Review Report Card and individual state report recommendations on clinician skill-building.
- Identify appropriate organization-wide training opportunities like CAPC Membership.
CAPC’s tools, training, and technical assistance can play a significant role in any statewide quality improvement efforts. The individual state reports highlight the number of organizations that already have access to CAPC training in communication skills, pain and symptom management, supporting family caregivers, and building new palliative care programs. Palliative champions can leverage this access in any education initiatives or new requirements, and may even consider working with policymakers, funders, or other stakeholders to support expanded CAPC access.
Do you have additional suggestions, or questions, on how to leverage the 2019 State-by-State Report Card? Email [email protected] to share your thoughts!

