Calling All Palliative Care Leaders: We Asked, You Answered

Today’s palliative care leaders are responsible for high-quality care delivery – and so much more. Whether it’s contracting with health plans, demonstrating impact on your organization’s quality measures, partnering with other service providers, developing strong teams, or identifying your highest-risk patients, palliative care leaders have their hands full.
CAPC is committed to supporting palliative care leaders.
In May 2019 we surveyed leaders working in the field about what keeps them up at night, and what we can do to help. With generous support from the Cambia Health Foundation, CAPC is using survey feedback from palliative care leaders to develop new tools, support resources, and networking opportunities. This blog post outlines the outcomes of the survey.
Who responded to the survey?
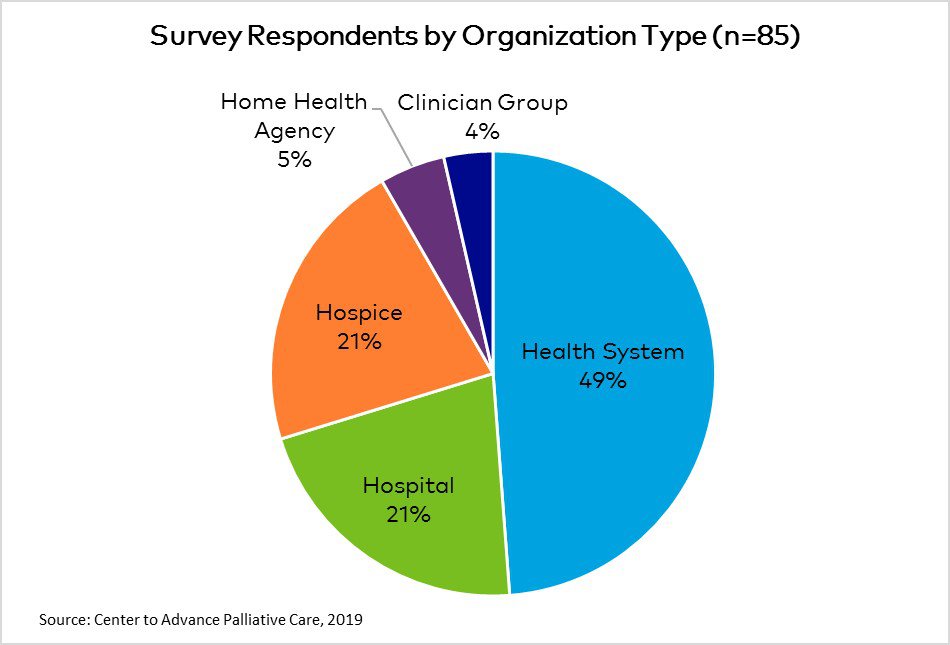
Those that responded to the survey include palliative care leaders representing health systems, hospitals, and community organizations responded to CAPC’s request for information. The teams represented in the survey provide palliative care services in hospitals, patient homes, clinics, SNFs, LTACs, or ALFs.
The largest portion of survey respondents lead palliative care programs (52 percent), while others are palliative care clinical leaders, business or administrative leaders within their organizations, or oversee a component of their organization’s palliative care services.
Level of Palliative Care Leadership Experience
Respondents ranged from being new to positions of leadership, to having 15+ years of leadership experience in palliative care.
| Leadership Stage | Percentage of Survey Respondents |
|---|---|
|
Aspiring leader: Have taken on formal or informal team or process leadership responsibility and wish to develop into a more formal leadership position |
11% |
|
New or early-stage leader: In my first leadership role, or a clinician or administrator with some leadership experience but new to leading a palliative care program. Would benefit from core leadership skill building. |
21% |
|
Mid-stage leader: 3+ years of palliative care program leadership experience. Wish to refine or refresh leadership skills. |
37% |
|
Advanced-stage leader: Have solid leadership experience and am in a position of overseeing a complex palliative care program at an enterprise or system-level that requires high-level leadership skills. |
26% |
| Other | 5% |
What Palliative Care Leaders Want
In our survey, CAPC asked palliative care leaders which leadership skills they most want to strengthen, and which challenges they face within several domains of leadership. Here is what we found.
Partnership Development
77 percent of survey respondents said that they wanted to strengthen their partnership skills, and 36 percent report that this is the leadership domain in which they have the most need for support. Included in this domain are contracting skills, as well as best practices for partnering with health plans, referring providers, and philanthropists.
What challenges do leaders face in developing partnerships?
- Educating referrers about patient eligibility criteria
- Navigating competition
- Leveraging existing initiatives and/or contracts to integrate palliative care services across the health system
- Billing and credentialing when providing services for partner organizations
- Identification of – and outreach to – potential payer partners
- Identifying strong partners in the context of limited resources
- Making time to develop and nurture partner relationships
- Accessing organizational support for contracting
- Operationalizing the different requirements of different partners
Administration Skills
67 percent of respondents would like support to develop their administration skills, with 35 percent reporting that this is the domain in which they would most like to develop their leadership capacity. This domain includes skills to conduct a needs assessment, develop strategic plans and business plans, measure palliative care program effectiveness and demonstrate value, and manage program budgets.
What administrative challenges do leaders face?
- Creating time for program administration
- Demonstrating value in an RVU-driven culture
- Making strategic growth decisions
- Navigating organizational politics and responding to service requests from leadership
- Collecting data efficiently
- Educating key stakeholders about palliative care
- Building the budget
Personnel
53 percent of those surveyed would like support in the area of personnel, including developing staffing plans, hiring and onboarding, measuring staff performance, leading an interdisciplinary team, and promoting effective relationships between clinical and administrative leaders.
What personnel challenges do leaders face?
- Setting standards for job performance
- Recruiting clinicians
- Clarifying roles
- Addressing dysfunctional team dynamics
- Improving retention
- Cultivating resilience
Communication
46 percent of survey respondents want support to develop effective communication among teams and across disciplines, give and receive feedback, diagnose and address communication breakdowns, and manage conflict.
What communication challenges do leaders face?
- Fostering inter-professional practice and sound team communication practices
- Balancing individual communication styles on the palliative care team
- Managing conflict
- Translating the value of palliative care for diverse stakeholder audiences
- Collaborating with referring specialists
Cultivating Leadership Styles and Roles
49 percent of respondents say they want to build their leadership capacity by understanding different leadership models, learning to lead through change, strengthening their decision-making and prioritization skills, and developing approaches to build organizational support for their programs.
What are the challenges in navigating one’s leadership role?
- Making time for transformation leadership–beyond managing day-to-day operations
- Navigating relationships with stakeholders who have different or conflicting visions
- Prioritizing and delegating tasks
- ‘Owning’ and leveraging personal leadership strengths
- Elevating one’s leadership status within the organization
Strengthening Leadership Skills
How can palliative care leaders strengthen their skills?
In addition to the toolkits linked above, CAPC will launch a new leadership initiative in January 2020. “Leadership Roundtable: Tackling Pressing Problems” will offer a year-long series where a panel, composed of seasoned palliative care leaders representing a variety of program models, will present a webinar every other month to address the most pressing topics from CAPC’s survey. Virtual Office Hours will follow each webinar, with panelists responding to real-time questions on leadership issues. CAPC thanks the Cambia Health Foundation for making this work possible.
Stay tuned for these highly interactive leadership development sessions, and for an advance look attend the National Seminar in Atlanta this November to hear a keynote from the new CAPC Leadership Panel. As always, dial into Virtual Office Hours for real-time coaching from national experts on key leadership topics.

