Part 1: Buprenorphine as an Essential Tool for Palliative Care Clinicians

Case Study + Introduction
Meet Mr. D, a 54-year-old male with stable Stage IV lung cancer who is under active treatment with immunotherapy. He has suffered from chronic pleuritic pain since a surgical resection 3 years ago, and has used a stable dose of a fentanyl patch and oxycodone (200 mg morphine equivalents daily) for pain management for the past several years. In recent months, Mr. D has developed opioid misuse behaviors (e.g. running out early, self-escalating doses, concurrent alcohol use, and presenting to the emergency room for refills).
Mr. D meets criteria for an opioid use disorder (OUD) (expand Figure 1 below). Therefore, he and his palliative care team make a shared decision to initiate buprenorphine/naloxone (prescribed by a clinician with a DEA registration).
Within a few weeks of starting on buprenorphine/naloxone, Mr. D achieved pain control on a dose of 4 mg buprenorphine/1 mg naloxone (three times/day). He has been doing well on this regimen – with stable behaviors, improved pain, and better quality of life. Intermittently, a full-opioid agonist is added to his regimen as needed, to help with pain from a chest tube. He recently told his palliative care team, “My life has improved so much this past year. I feel physically and emotionally better than I have in years, even though I am living with Stage IV cancer.”
Figure 1: Select Opioid Use Disorder Criteria (expand +)
The 4 C's can be a helpful mnemonic for 12 DSM diagnostic criteria that establish both the diagnosis of OUD and the severity (from mild, moderate, severe). In this case, Mr. D presents with:
4 C: Craving
DSM-5 Criteria: Strong desire or urge to use an opioid
Possible manifestation of OUD: Patients can often understand this term and respond to questions about craving directly; note that pain can be a sign of craving
4 C: Control (lack of)
DSM-5 Criteria: Use of an opioid in increased amounts or longer than intended
Possible manifestation of OUD: The patient is asked to limit their opioid quantity to 5 per day, and is given a one-week prescription that reflects this amount, but still runs out 3 days early
4 C: Consequences
DSM-5 Criteria: Continued opioid use despite problems socially, interpersonally, medically
Possible manifestation of OUD: Strained relationships with family and clinicians surrounding opioid use; continued use despite being told by clinicians that they are being physically or psychologically harmed by the opioid
4 C: Compulsive Use
DSM-5 Criteria: Use of an opioid in physically hazardous situations
Possible manifestation of OUD: Self-escalation of opioid dosing; when asked, patient may say take the opioid “without even thinking about it”
For more on possible manifestations, click here.
As palliative care clinicians, these are words we like to hear. We strive to achieve symptom control and quality of life for all our patients and are always looking for new tools that strike the balance between efficacy, safety, and versatility. Buprenorphine has the potential to be an important option.
In this two-part blog post, we explore the ways buprenorphine can help people living with serious illness—especially those who experience a range of both pain and opioid use challenges. In part one, we provide background on buprenorphine, including its pharmacology. Later, in part two, we discuss considerations for prescribing, how to prescribe, and potential barriers to use.
The Importance of Buprenorphine as an Analgesic
Buprenorphine can be an effective analgesic with fewer adverse effects than traditional opioid agonists, such as morphine or oxycodone. Some advantages of prescribing buprenorphine for pain include:
- Decreased risks of respiratory depression, sedation, euphoria, craving, dysphoria, hyperalgesia, and constipation; and other GI side effects
- Less effect on the hypothalamic pituitary axis, thus carrying less risk for hypogonadism and its associated complications, such as sexual dysfunction, decreased libido, and osteopenia
- An association with less QTc prolongation, arrhythmia, and sudden death, when compared to methadone
- Safe for use in renal failure or during dialysis, and well tolerated in patients with liver disease
- If buprenorphine doses have been stable, co-prescribing with short-acting opioid agonists can be done safely, such as for post-operative pain, as Mr. D’s palliative care team did, in the case presented earlier
How Buprenorphine Works
Given the advantages of buprenorphine—and we would argue that these advantages are particularly germane in individuals at the intersection of serious illness and chronic pain—why isn’t it more widely used in palliative care settings? The three main reasons may be a lack of clinician familiarity, relative expense, and requirements for prior authorization. However, we routinely use buprenorphine in our palliative care practices and help others get started. It can be done. Let’s get more familiar with buprenorphine and discuss how it works.
Buprenorphine Pharmacology
Most clinicians know buprenorphine for its efficacy in the treatment of OUD, including reduction in opioid mortality and illicit opioid use. However, buprenorphine was originally developed as an analgesic—relieving pain by acting on the central nervous system. Because of its unique properties, buprenorphine is effective for both pain and OUD.
- Buprenorphine acts as a partial agonist at the µ opioid receptor; an antagonist at the kappa and delta-opioid receptors; and a full agonist at the opioid receptor-like receptor.
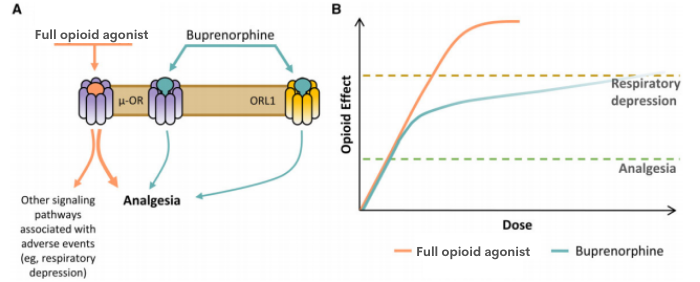
- Its strong affinity for the µ opioid receptor and slow dissociation may provide sustained analgesia at relatively low doses. There has been concern that as a partial µ agonist, buprenorphine may have limited potency, but evidence suggests it can provide analgesia similar to “full” opioid agonists (e.g., morphine, oxycodone).
- Due to buprenorphine’s increased spinal cord activity and reduced activity in the brain, there is a decreased risk for respiratory depression and hyperalgesia.
- Antagonist activity at the kappa and delta-opioid receptors appears to lessen craving, sedation, and dysphoria.
- Additionally, kappa antagonism may improve the stability of comorbid mental health conditions, such as anxiety and depression
We will discuss the details of prescribing in part two of this blog post, but it is essential to highlight that buprenorphine can now be prescribed without an X waiver. The Omnibus bill eliminated the federal requirement for clinicians to submit a Notice of Intent (have a waiver) to prescribe medications like buprenorphine in order to treat opioid use disorder (OUD). Clinicians have always been able to prescribe buprenorphine for pain, even without a waiver.
All clinicians with a current DEA registration, including Schedule III authority, are now permitted to prescribe buprenorphine for pain and/or opioid use disorder in their practice, subject to applicable state law.
Read on in part two, where we discuss when to consider prescribing buprenorphine for your patients, how to prescribe, and potential barriers.
Take CAPC's new courses for comprehensive clinical training in chronic pain management, risk mitigation, assessing opioid misuse, and assisting with access to treatment for opioid use disorder (OUD) for patients living with serious illness.
Get StartedEdited by Melissa Baron. Clinical review by Andrew Esch, MD, MBA.
*This blog post was updated on 3/14/2024 to remove references to the previous X-Waiver requirement.

