The Case for Better Behavioral Health Integration in Serious Illness Care Settings

A vast body of research shows that many people living with serious medical illnesses like cancer, stroke, heart disease, COPD, end stage renal disease, chronic neurologic/neurodegenerative disease, and dementia also suffer from co-morbid behavioral health issues. (See each individual link for associated studies.)
A vast body of research shows that many people living with serious medical illnesses [...] also suffer from co-morbid behavioral health issues.
These can be pre-existing issues (e.g., depression), exacerbations of pre-existing issues (e.g., worsened depression in the setting of illness-related stressors and medications), or de novo issues (which could include adjustment disorders, responses to financial and role-change stress, medication-related mood or psychotic symptoms, or cognitive impairment.) Patients may be (though more often, are not) receiving some kind of behavioral health support at a cancer center, an ALS center, an HIV clinic, or outpatient setting, but even when available these interventions are time-limited or poorly aligned amidst myriad scenarios.
Meeting Behavioral Health Needs
Addressing behavioral health issues in the light of evolving conditions and stages of serious illness, different care settings, changing needs, and potential shifts in the treatment team requires a comprehensive and flexible system that involves intensive coordination with all involved health professionals, and friends and family. This includes behavioral health, non-behavioral health, family, and other caregivers across the entire duration and care continuum of a serious illness. In addition, patients at the interface of behavioral health and serious illness care almost always require additional social services that go beyond the immediate clinical realm.
However, along with the acknowledgement that these patients “should” get their needs addressed, come some fundamental questions:
Who
- Who needs care?
- Who provides it (and in what setting)?
- Who will pay for it?
What
- What care services are needed (i.e., physical/behavioral health care, social services)?
- What are the care navigation/coordination needs?
- What are the workforce needs to provide the necessary range of skills?
How
- How are patients with these needs identified?
- How can care services be delivered in a coordinated way?
- How should these services be supported (Health IT, payment models, accountability mechanisms across the care continuum)?
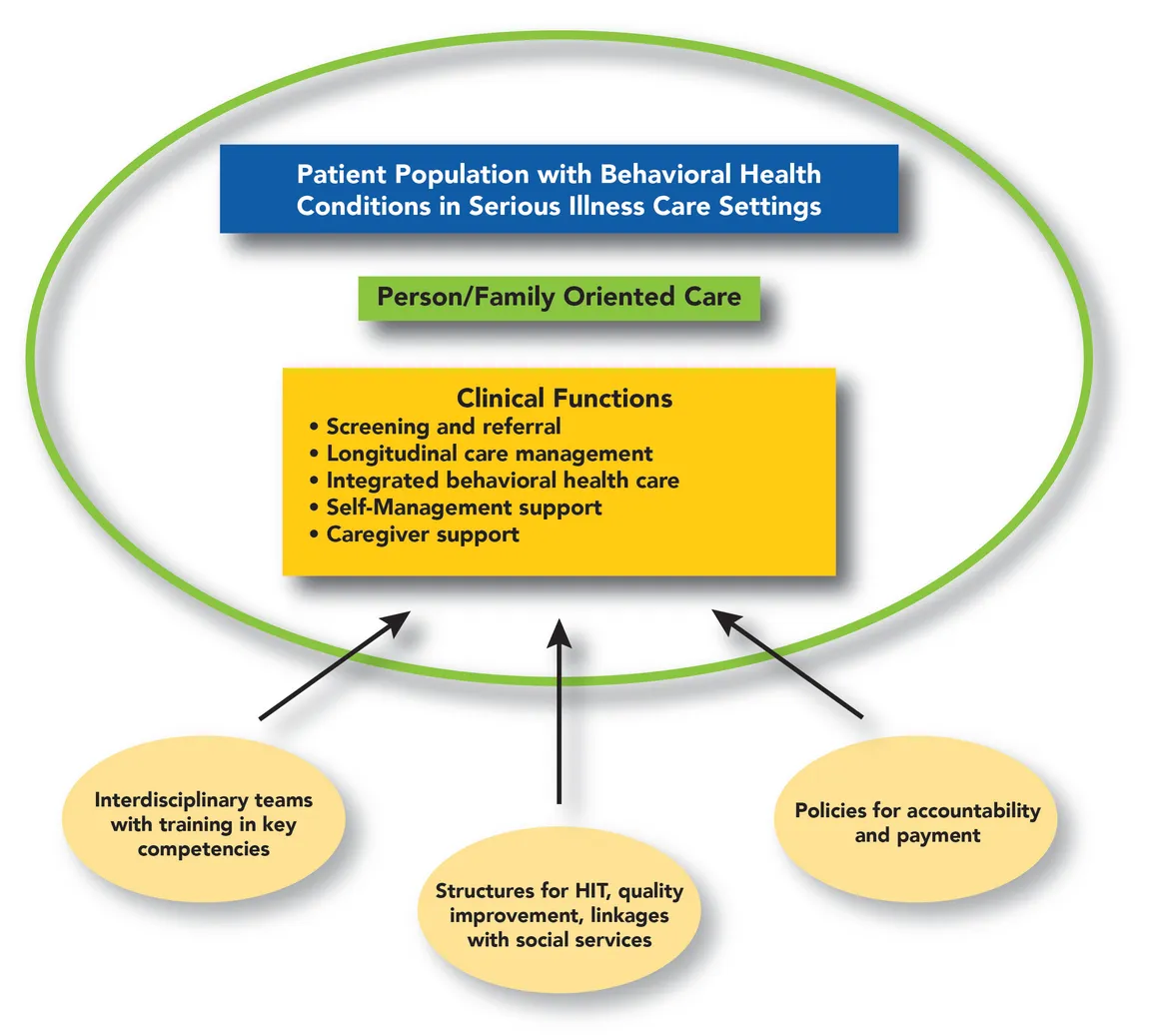
To address these questions, a team of researchers at Columbia University/New York State Psychiatric Institute developed a Behavioral Health-Serious Illness Care (BH-SIC) model, which identifies a set of 5 key components, based on 13 domains and 16 sub-domains. The domains can be adjusted and applied to different settings and stages across the behavioral health/serious illness care continuum to address issues of person/family-oriented care, clinical functions, workforce, structural requirements (e.g., Health IT, systematic quality improvement strategies), and broader health policy issues (e.g. alternative payment models).
Recommendations for the Field
While this model offers maximum flexibility for application and implementation of its key components, first practical steps that we recommend taking include:
- Getting buy-in from organizational and clinical leadership, as well as staff for behavioral health integration across clinical activities;
- Identifying immediate steps that could be taken within your organization – e.g., staff training to raise awareness of behavioral health issues among patients (‘low-hanging fruit’).
More advanced strategies would involve an assessment of gaps and needs at the clinical, organizational, and financial level to advance behavioral health integrations and scale up integration efforts.
Key Concepts of the Behavioral Health-Serious Illness Care (BH-SIC) Model
Central to the proposed integrated BH-SIC model is care that reflects the values, preferences, and concerns of the patient and identified family. Communication and acknowledgement of their needs and preferences should be proactive and continuous, even as personnel or settings change throughout the span of the illness.
Central to the proposed integrated BH-SIC model is care that reflects the values, preferences, and concerns of the patient and identified family.
Clinical functions as defined in our model encompass and go beyond psychotherapeutic and psychopharmacological care. Additional clinical functions include recognizing behavioral health needs, connecting the patient to the appropriate care, longitudinal follow up, coordination between behavioral health and non-behavioral health personnel, and support for family members and other caregivers.
Staffing and Support for the BH-SIC Model
The ideal workforce to support the model consists of a multidisciplinary team whose members have cross-trained sufficiently in order to recognize when another discipline is needed, and to provide in-the-moment services while additional help is arranged. Realistically, few if any existing teams caring for people with serious medical illness are fully staffed with cross-trained psychiatrists, social workers, psychologists, and others trained and expert in behavioral health. Recognizing this gap, our research team developed a set of core clinical team competencies (basic, intermediate, and advanced) based on the BH-SIC model to scale up and upskill the workforce at this interface (see Table 1 below).
Table 1: Core Clinical Team Competencies Based on the BH-SIC Model
| Clinical Domain |
Competencies (1. Basic; 2. Intermediate; 3. Advanced) |
|---|---|
| Communication, teamwork, and shared decision making |
1. Communicate appropriately and respectfully on advance care planning and decision-making 2. Effectively lead discussions about advance care planning and decision-making 3. Employ advanced techniques and train staff in these communication techniques |
| Case finding, screening, and referral to care |
1. Be aware of symptoms of common behavioral health conditions that necessitate further evaluation 2. Conduct appropriate, operationalized, evidence-based behavioral health screening and know how to escalate care (see Table 2) 3. Conduct in-depth behavioral health evaluation and facilitate and track referrals |
| Longitudinal care management and crisis management |
1. Recognize variation, and changes in symptoms and needs associated with behavioral health and serious illness; apply strategies to prevent/address crises 2. Identify and triage behavioral health/serious illness care crises across care settings 3. Coordinate longitudinal care needs across care settings/ teams |
| Integrated evidence-based and measurement-based care |
1. Assist patients and families to access evidence-based behavioral health treatments (incl. psycho-pharmacological and psychosocial interventions) 2. Directly provide evidence-based behavioral health treatments 3. Directly deliver stepped, measurement-based behavioral health care |
| Self-management support |
1. Be familiar with the concepts of patient activation, engagement, and self-management 2. Supply appropriate information/training materials 3. Deploy evidence-based techniques in self-management, engagement, and activation |
| Caregiver support |
1. Engage caregivers as shared partners in care 2. Understand the consequences of caregiver strain, identify signs, conduct needs assessments, and facilitate appropriate support 3. Deliver targeted interventions to alleviate caregiver strain |
| Responding to social determinants of health and linking to services |
1. Recognize impact of social determinants of health on health needs, engagement, and health outcomes 2. Provide basic information to patients and families about available services/options 3. Conduct screening for socioeconomic risks and connect patients/caregivers to services |
Table 2: Major Screens for Depression and Anxiety in Serious Medical Conditions
| Screening Tools* | |
|---|---|
| Depression |
• PHQ-2[1] is short but requires recall of the prior 2 weeks. • HADS-D is good for screening[2], superior to other screenings for depression[3]; but was least recommended in advanced CA and palliative care[4] and requires recall of the past week. • BDI is a valid screening tool in Parkinson’s[5], is more generalizable across cancer types and stages, has good indices for screening, but is long[4] and requires recall of the prior 2 weeks. |
| Anxiety |
• GAD-7 recommended[1] and requires recall of the past week. • HADS-A is good for screening[2], but performed worse than other HADS scales for screening[3] and requires recall of the past week. |
Additional Support Mechanisms
Other support mechanisms for the model involve enabling changes at the policy level. The implementation and delivery of integrated evidence-based psychopharmacological and psychosocial behavioral health care outlined in our model requires not only reliable financing but an improved accountability and quality measurement infrastructure – i.e., a) integration of behavioral health symptom monitoring data systems into electronic health records; b) adoption of measurement approaches that support accountability for the quality of care delivered; and, c) formalized linkages to social services (housing, transportation, food).
Routine uses of validated quality measures are essential to guiding systematic quality improvement efforts and tying payments to quality of care, rather than volume. However, the continuing lack of suitable quality measures (structure, process, and outcomes) at this interface poses challenges not only to the delivery of integrated care services, but also to the ability to pay for these kinds of services.
Payment
Similar to other integrated, patient-centered care models, our model requires payment that reimburses all aspects of care, including identification and treatment of behavioral health conditions, care coordination, and meaningful and sustained connection to social services (e.g., home support services, food, housing, transportation etc.). In addition, routine uses of validated quality measures are essential to guiding systematic quality improvement efforts and tying payments to quality of care, rather than volume. As noted above, actionable and feasible quality measures are prerequisite to payment under emerging value based payment models.
A novel payment model, recently introduced by CMS attempts to address this gap: the Primary Care First - Seriously Ill Population model was informed by models proposed by both the American Academy of Hospice and Palliative Medicine (AAHPM) and the Coalition to Transform Advanced Care (C-TAC). This model aims to transform care for high-need, high-risk patients through payment strategies that support effective, high-value care, and improve provider accountability. For more information, the Center to Advance Palliative Care (CAPC) summarized it in a recent blog post.
In Conclusion
The BH-SIC model’s components and potential barriers to implementation are described in detail in a special article, published in the Journal of Pain and Symptom Management. An extensive exploration of the scope of the problem, the development of the BH-SIC model, and the model itself are detailed in the full study report.
Since the original design of this model, a major world event occurred and is still unfolding. The ongoing COVID-19 pandemic, with its heightened psychosocial stressors and disruption of support systems, has not only created increased demand for behavioral health services, but also highlighted the unmet needs of individuals with behavioral health issues (with and without the virus) — and the siloed organizational, delivery, and funding structures of the US health system. Using flexible approaches to integration of BH care, and building robust integrated systems supported by adequate and sustainable funding is very important to help health systems better mitigate the impact of additional major challenges in times of crisis.
Endnotes
-
Andersen, B.L., et al., Screening, assessment, and care of anxiety and depressive symptoms in adults with cancer: an American Society of Clinical Oncology guideline adaptation. Journal of clinical oncology : official journal of the American Society of Clinical Oncology, 2014. 32(15): p. 1605-1619.
-
Mitchell, A.J., Short screening tools for cancer-related distress: a review and diagnostic validity meta-analysis. Journal of the National Comprehensive Cancer Network : JNCCN, 2010. 8(4): p. 487-494.
-
Vodermaier, A. and R.D. Millman, Accuracy of the Hospital Anxiety and Depression Scale as a screening tool in cancer patients: a systematic review and meta-analysis. Supportive care in cancer : official journal of the Multinational Association of Supportive Care in Cancer, 2011. 19(12): p. 1899-1908.
-
Wakefield, C.E., et al., Patient-reported depression measures in cancer: a meta-review. The lancet. Psychiatry, 2015. 2(7): p. 635-647.
-
Schrag, A., et al., Depression rating scales in Parkinson's disease: critique and recommendations. Movement disorders : official journal of the Movement Disorder Society, 2007. 22(8): p. 1077-1092.

