Positive Impact of Palliative Care Education on ICU Nurses

An estimated one in five Americans dies after admission to an intensive care unit (ICU),[i] yet the palliative care needs of ICU patients and their families often go unmet. According to one recent estimate, less than five percent of ICU patients receive specialist palliative care.[ii] The active engagement of bedside nurses is a prerequisite for the sustained integration of palliative care in ICU settings. Palliative care support also helps ICU nurses manage the emotional demands of their job. A recent surveyof ICU bedside nurses, however, identified inadequate training and skills in palliative care as key barriers to nurses’ involvement in palliative care communication.[iii]
Upon reading about the results of this survey, Jeffrey Marsh, MD, medical director of hospice and palliative care at Aultman Hospital in Canton, Ohio, proposed asking this question: What is the comfort level with and level of participation in palliative care discussions by Aultman’s ICU nurses? For background, Aultman is a 682-bed tertiary care hospital employing approximately 250 ICU nurses, who work in four ICUs – medical, surgical, cardiovascular, cardiac care, and a long-term acute care specialty unit.
Understanding nurses’ perspectives, identifying perceived barriers
With the goal of better understanding bedside nurses’ perspectives on their involvement in palliative care communication, and to identify the perceived barriers to providing palliative care information to ICU patients and their families, in 2017 the Aultman team conducted a modified replication study, using an anonymous survey.
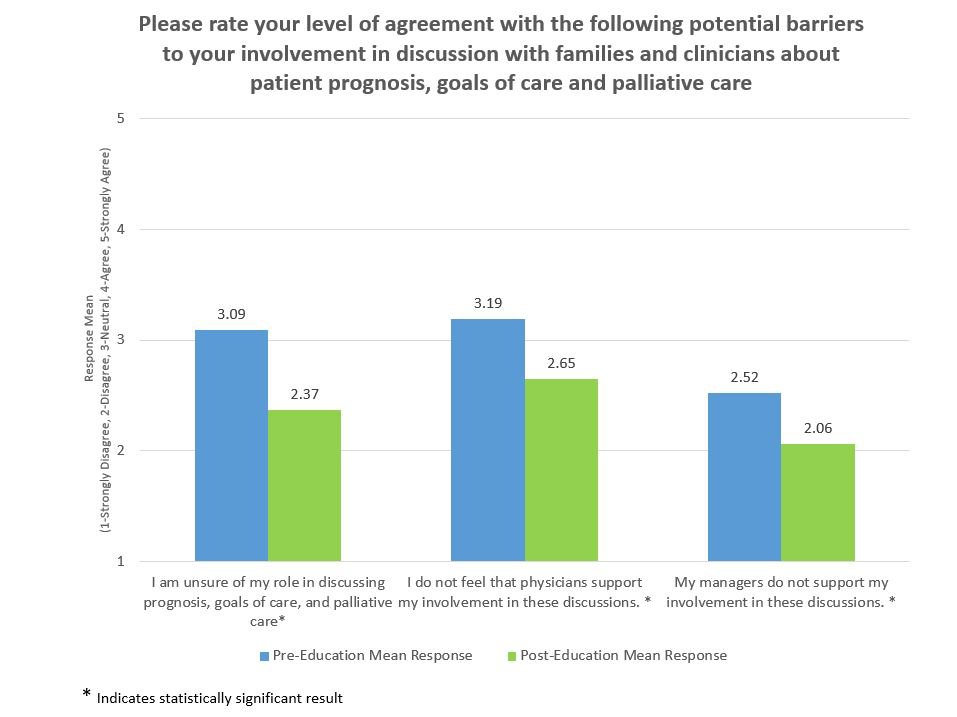
Fifty-nine bedside nurses working in Aultman’s ICUs participated in the survey. Respondents believed they were able to discuss goals of care with patients and families (x=3.58/4), but were often unsure of their role in discussing palliative care (x=3.09/5). Additionally, the nurses felt uncomfortable initiating a conversation if the physician had not discussed prognosis with the family.
A multimodal education program for ICU nurses
These baseline data were used to develop a multimodal palliative care education program for Aultman’s ICU nurses implemented between January and April of 2018. In Part 1 of the program, which was aimed at improving participants’ basic understanding of palliative care and its goals, nurses completed the CAPC online course An In-Depth Look At Palliative Care And Its Services.
Part 2 consisted of a 30-minute live presentation developed by Aultman’s palliative care clinical nurse specialist, Tammie Thompson. Topics addressed included the differences between the palliative care and hospice programs at Aultman, therapeutic communication techniques, and the role of the bedside ICU nurse in palliative care discussions. Participants also received a pocket resource card that offered reminders about therapeutic communication techniques and references to resources for palliative care discussions.
“One of the biggest points I took away from the palliative care class was to advocate more to get palliative care involved in chronic illnesses and not just for end-of-life situations.”
In total, 215 ICU nurses completed the two-part education program. Verbal feedback indicated that they felt an increased urgency to involve palliative care at earlier stages of care and that they had greater clarity about their role in these important conversations with patients and families.
Medical intensive care registered nurse Lani Lowery commented, “One of the biggest points I took away from the palliative care class was to advocate more to get palliative care involved in chronic illnesses and not just for end-of-life situations.”
Emily Klusty, also a registered nurse in the medical intensive care unit, said, “The class positively impacted my knowledge by helping me understand how to better educate my patients and their families about the difference between palliative care and hospice care.”
Phase 2: Follow-up survey
In the second phase of the initiative, we surveyed ICU bedside nurses who had completed the education program to determine whether it had decreased perceived barriers and improved their involvement in palliative care communication. Thirty-two nurses responded to this second survey. (Because both surveys were anonymous, it is not possible to determine the extent of overlap, if any, between respondents to the two surveys.)
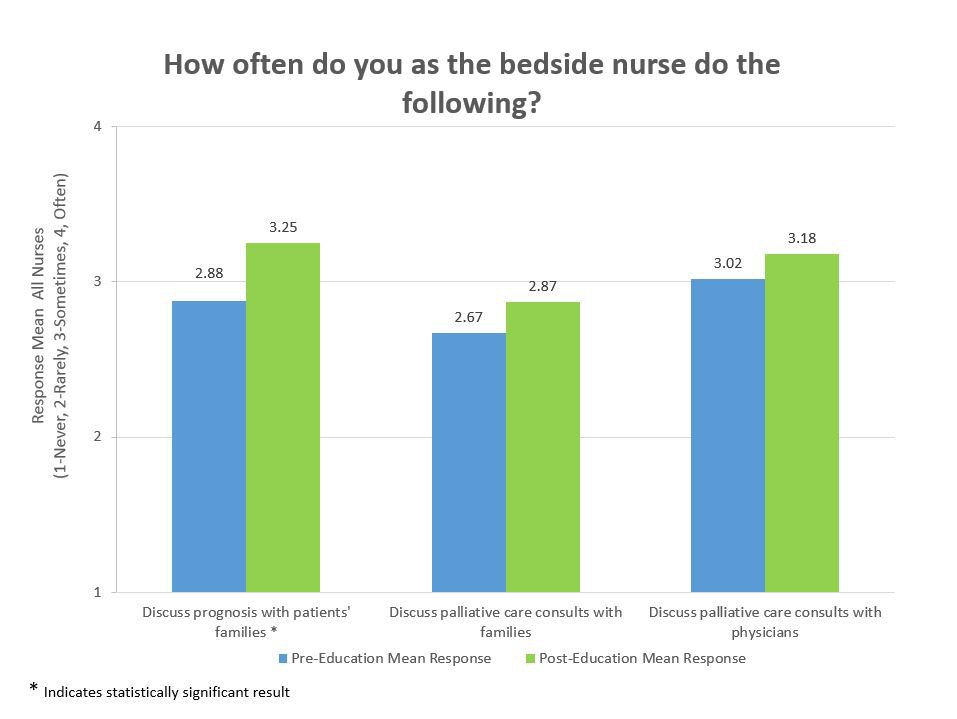
Comparison of participants’ mean pre- and post-education responses to the second survey showed that the education program enhanced ICU nurses’ perception of their palliative care abilities. A positive change in perceptions related to palliative care was seen in the responses to 88% of the questions; on four questions, the pre-post change was statistically significant. (See figures below for two of the questions.)
We recognized that due to high nursing-staff turnover in the ICUs, it was important to continue to offer the palliative care education program to new nursing staff. The 30-minute presentation developed by Thompson was recorded and is now available online to all nursing staff at Aultman and the two-part palliative care education program is available to all new ICU nurses to view and learn through orientation or as a continued resource.
Advancing the practice of palliative care in our ICUs
Nurses have reported that they appreciate receiving information about a topic that can be confusing to many who are not in the palliative care field. Feedback from the education program revealed that many of the nurses were receptive to ideas about how to initiate goals-of-care conversations and ask appropriate questions in order to advocate for patients and their families. Additionally, nurses indicated in their responses to the follow-up survey that the education program had enhanced their confidence in their ability to communicate patients’ and families’ expressed needs and wishes, both to their fellow nurses and to the intensivist physicians who manage the patients’ care. (In Ohio, palliative care consultations require a physician order.)
Nurses have reported that they appreciate receiving information about a topic that can be confusing to many who are not in the palliative care field.
By asking a few simple questions in a structured fashion (e.g., “What do you know about palliative care?”, “How comfortable are you with discussing this topic with patients?”), we were able to educate and encourage our ICU nursing staff, and to advance the practice of palliative care in our ICUs by meeting with staff and educating to their specific role. In addition to the changes mentioned earlier to implement training in the Aultman ICU, some units now include palliative care modules – developed by CAPC and those developed by the American Association of Critical Care Nurses – in nurses’ annual required education. We continue to educate new nursing staff and provide clarification where needed to ensure that our patients are receiving the best possible care.
CAPC Resources
Are you looking to integrate palliative care into the ICU at your hospital? Review CAPC's toolkit, Palliative Care Practices in the ICU, which was developed in an effort to increase access to palliative care services for patients (and their families) receiving care the ICU. The toolkit includes the following resources:
- An introduction to palliative care in the ICU, including the "what and why" of ICU palliative care, including standards for ICU palliative care and how to make the case
- Program design, including guidance on model design and tools for identifying patients in the ICU who would benefit from palliative care
- Sample policies and clinical tools for both palliative care and ICU teams to assess need, conduct family meetings, and provide services in the ICU
- And more
Click here to access to toolkit
Endnotes
-
[i] Angus DC, Barnato AE, Linde-Zwirble WT, et al. Use of intensive care at the end of life in the United States: an epidemiologic study. Crit Care Med. 2004 Mar;32(3):638-43.
[ii] Wysham NG, Hua M, Hough CL, et al. Improving ICU-Based Palliative Care Delivery: A Multicenter, Multidisciplinary Survey of Critical Care Clinician Attitudes and Beliefs. Crit Care Med. 2017 Apr;45(4):e372-e378. doi: 10.1097/CCM.0000000000002099.
[iii] Anderson WG, Puntillo K2, Boyle D, et al. ICU Bedside Nurses' Involvement in Palliative Care Communication: A Multicenter Survey. J Pain Symptom Manage. 2016 Mar;51(3):589-596.e2.


