Integrating Palliative Care in the Emergency Department: A Paradigm Shift
The Emergency Department (ED) is the domain of life saving, life-sustaining interventions for the seriously ill, but for some patients it may also provide an opportunity to expand the focus of medical care to include symptom relief and improving quality of life. This is one ED’s journey: Morristown Medical Center.
People enter the ED in search of help when a medical or surgical emergency arises. They arrive at our doors via helicopter, ambulance, wheelchair, or under their own steam—suffering from pain, respiratory distress, with symptoms of a stroke or heart attack, or as the victim of a motor vehicle accident. These are the patients that ED physicians and nurses have been trained to stabilize and resuscitate; this is where the adrenaline kicks in and the team jumps into action. While ED staff are trained to save lives, all too often they are also faced with situations where the usual approach—do everything and anything to prolong life—may add to suffering with little to no likelihood of benefit.

Not Our Business – Or Is It?
In 2017, over 136 million visits were made to EDs nationwide; as the population ages, many ED patients will be living with one or more serious, usually chronic, illnesses, with symptoms and functional decline severely reducing quality of life. As an entry point to care, the ED is uniquely positioned to identify the real needs of the patient and the family, and to reorient the services offered to meet those needs. Historically, however, ED clinicians have avoided goals of care conversations about what is most important to the patient and family, assuming these were the domain of the primary care clinicians or their hospital colleagues.
As an entry point to care, the ED is uniquely positioned to identify the real needs of the patient and the family.
ED staff, in turn, suffered from varying degrees of moral distress and frustration at their inability to meet their patient’s true needs in situations where the usual approach to disease treatment appears to be doing more harm than good—by adding stress and suffering without meaningful gain in survival, function, or quality of life.
Background: Palliative Care in the ED

In 2011, the Center to Advance Palliative Care recommended that every hospital develop a systematic approach to ensure identification of patients at high risk for unmet palliative care needs; the Emergency Nurses Association (ENA) supports this recommendation and included it in its position statement, which calls for ED nurses to lead collaborative efforts for providing quality palliative care. Due to these efforts (and others in the field), palliative care is now a recognized sub-specialty in emergency medicine.
Palliative care is now a recognized sub-specialty in emergency medicine.
Moving Forward: Nurses Integrate Palliative Care
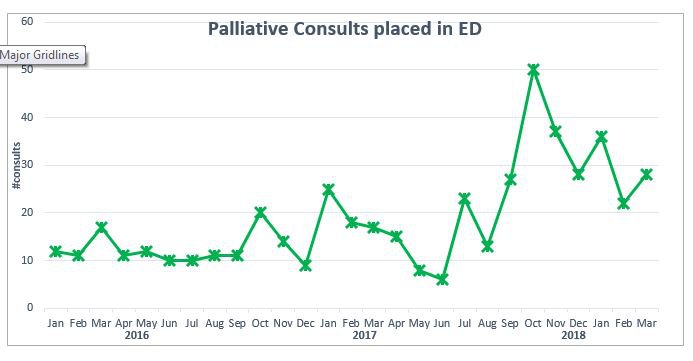
In late 2016, our ED began to explore how to more fully integrate palliative care into our practice. Previously, palliative care consults were requested very infrequently in the ED; they were reserved for dying patients appropriate for hospice care. The advent of a new eleven bed palliative care unit—and the hiring of additional palliative care clinicians—provided the impetus needed to move the initiative forward.
Goals of project:
- Improve comfort level of ED nurses and physicians in talking with patients and families about achievable and meaningful goals for care, especially in stressful decision-making situations.
- Develop an easy-to-use screening tool to identify patients who would benefit from a palliative care consult, and use this to initiate an early consult while the patient is still in the ED.
- Increase utilization of palliative care services to more closely align care delivery with patient and family goals of care.
- Secondary objectives include decreased ED, hospital, and ICU length of stay, improving patient, family and clinician experience, and improving patient quality of life.
Implementation:
- An interdisciplinary group, including nurses and physicians, developed a set of evidence-based screening criteria and an algorithm to identify patients who might benefit from earlier palliative care involvement.
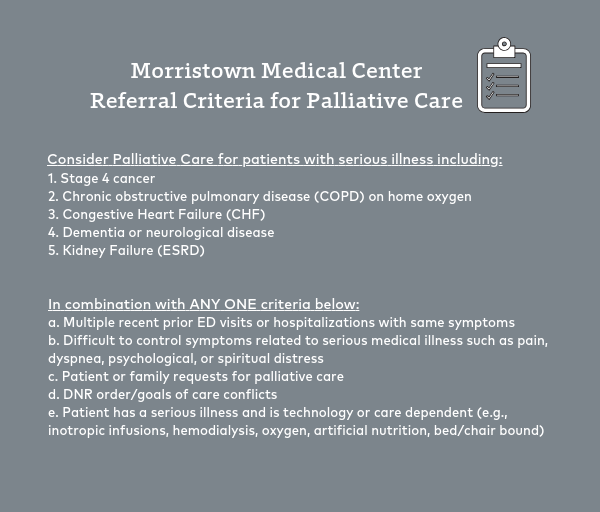
- The screening tool was added to the nurse assessment in the electronic health record (EHR), together with a standing order protocol, that supported ED nurses in placing a palliative care consult for patients meeting the criteria.
- An educational plan was developed with both didactic and hands-on simulation to improve knowledge of palliative care and communication techniques. Staff honed their communication skills during interactive scenarios with a group of trained professional actors who played very realistic roles of patients and their families.
Results:
- In a post-implementation survey, staff reported increased confidence in initiating goals of care discussions with patients and families, and expressed interest in additional education on this topic.
- Since September 2017, an average of thirty-two palliative care consults have been placed per month, an increase of 400 percent over the prior months. Consults occur within 24-48 hours of ED arrival, compared to five to seven days, prior to initiative.
- The most common underlying diagnosis is cancer (36 percent), followed by stroke (21 percent) and heart failure (14 percent). Leading sources of symptom distress in this group are dyspnea, altered mental status, and pain.
- ED residents and physicians report satisfaction with a more streamlined process for ordering palliative care consults.
In Conclusion
The use of a screening tool as a basis for placing a palliative care consult for ED patients has resulted in a substantial increase in patients referred to the palliative care team. The majority were appropriate consults, supporting the ability of ED staff to use the screening tool as a basis for ordering palliative care consults.
Placing palliative care consults in the ED resulted in patients receiving palliative care services earlier in the treatment trajectory, rather than waiting for a crisis.
Placing palliative care consults in the ED resulted in patients receiving palliative care services earlier in the treatment trajectory, rather than waiting for a crisis. Earlier access resulted in earlier goals of care conversations, development of care plans matched to patient and family needs and priorities, and a better match of services to needs.
There has been a cultural shift within the ED regarding palliative care referrals, from “it’s not my job” to a recognition of the important role that palliative care can play in improving patient outcomes. Staff report a sense of accomplishment in providing care which better supports a patient’s needs and goals. During a recent educational session, nurses commented that the referral tool is a resource that truly helps meet the needs of patients and their families, that they would like more training, and that they wish more colleagues would employ the same approach.
There has been a cultural shift within the ED regarding palliative care referrals.
Additional Resources
CAPC members have access to a variety of patient identification and assessment tools in the hospital setting, which should be modified as appropriate to fit your setting and patient population.
