Spotlight on Pediatric Palliative Care: National Landscape of Hospital-Based Programs, 2015-16
Hospital administrators, policymakers, payers, and health professionals now recognize palliative care’s proven potential to improve care quality and clinical outcomes[1] while reducing costs.[2] This momentum is beginning to spread to the use of pediatric palliative care throughout the care continuum to meet the needs of infants, children, adolescents, and families coping with serious illness.
Until recently, pediatric palliative care programs have been most available in the hospital setting.[3] According to a 2013 study, 69% of responding children’s hospitals reported the presence of a palliative care team, but team staffing and capacity varied tremendously.[4] Now, many are expanding to provide perinatal palliative care services as well.[5] Most of these programs remain heavily reliant on making the case to hospital leaders for funding support, so program-level and comparative data are critical for developing, sustaining, and expanding these pediatric and perinatal palliative care services.
The National Palliative Care Registry™ was developed as an “open source” platform to support the field by promoting standardization and providing actionable data that palliative care programs can use to secure and expand resources for the delivery of high-quality palliative care. Key metrics include numbers of patient encounters, staffing models, diagnosis categories, referral sources, length of stay, and discharge status. The Registry is expanding to improve access to the national pediatric programmatic data necessary to drive standardization, quality, and access. The Registry is free and open to all palliative care programs, providing critical guidance for teams to consistently capture and compare operational information across the spectrum of hospital- and community-based service settings.
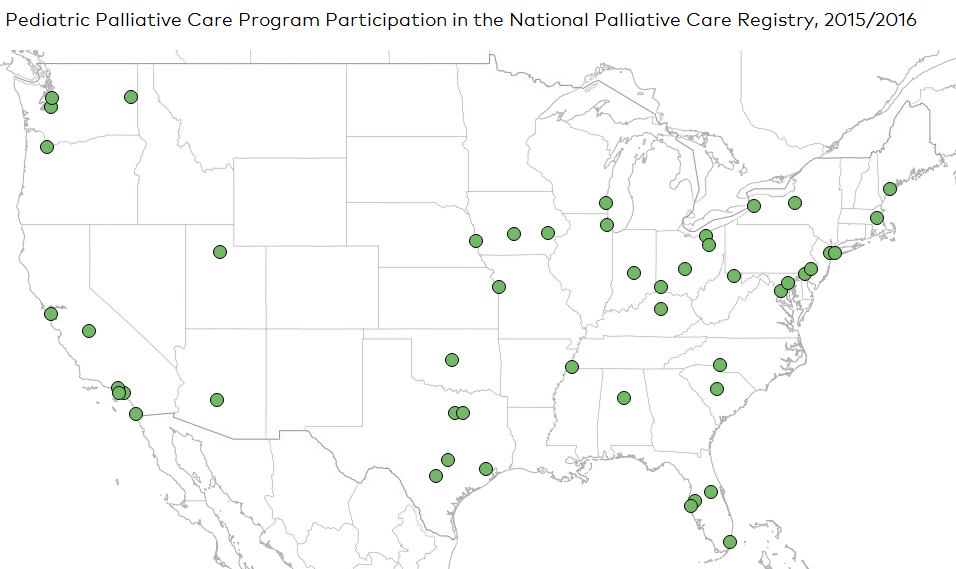
Fifty-two hospital pediatric palliative care programs participated in the National Palliative Care Registry™ in 2015/2016. Participating programs were predominantly in teaching (92%) and non-profit hospitals (81%). More than 90% (47 of the 52) of respondents were children’s hospitals, representing 42% of the estimated 112 children’s hospitals with palliative care programs in the U.S.[4] and 21% of the estimated 220 children’s hospitals in the U.S.[6] While the Registry doesn’t represent all pediatric programs in the United States, it provides a lens through which to examine the range of staffing and delivery models and their impact on number of children served.
Key findings from 52 Pediatric Palliative Care Programs:
1. Registry participation was highest in urban areas.
Almost all participating pediatric palliative care programs (84%) were located in urban areas. Additionally, twenty-seven states and Washington, D.C., were represented. Geographic locations of the participating pediatric palliative care programs are shown in the map below.
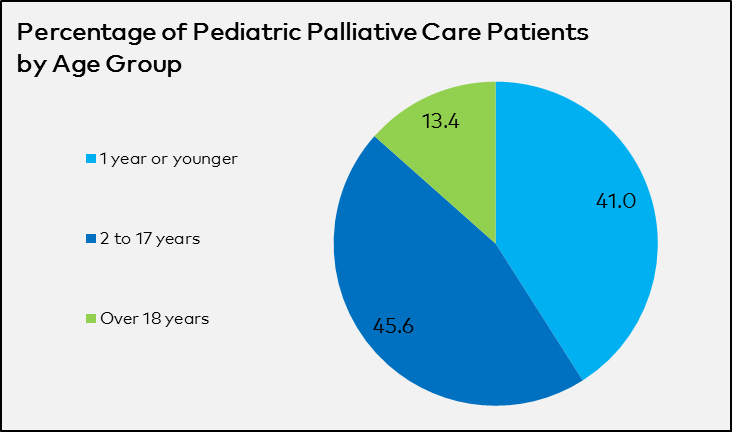
2. Pediatric palliative care programs provide care to patients of all ages and stages of development.
One quarter of pediatric palliative care programs provided palliative care to infants, children, and adolescents under eighteen years old only, while three-quarters of programs also provided palliative care to some young adults or adults. Additionally, about half of programs provided perinatal palliative care.
On average, 41.0% of pediatric palliative care patients were under one year of age, including perinatal patients, and 45.6% were between the ages of two and seventeen.
3. Pediatric palliative care programs see patients frequently throughout a hospitalization.
Palliative care service penetration is defined as the percentage of annual hospital admissions seen by the palliative care team. On average, pediatric palliative care programs saw 2.6% of annual pediatric admissions and newborns. Penetration among participating hospitals ranged from less than 1% all the way up to 15%.
Over the course of one year, pediatric palliative care programs provided an average of 235 initial consults and saw an average of 141 unique patients. pediatric palliative care team members provided an average of over 1,000 billable subsequent visits (by physicians and APRNs) and an additional unrecorded number of non-billable subsequent visits (by other team members including social workers and child life specialists).
This translates to an average of nearly five billable subsequent visits per initial consult, or over eight billable subsequent visits per unique patient, during the pediatric palliative care patient’s time in the hospital.
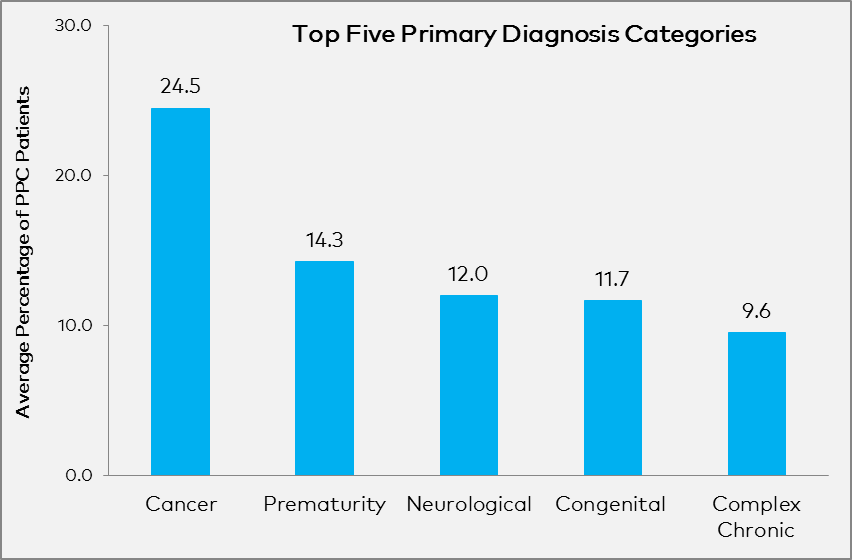
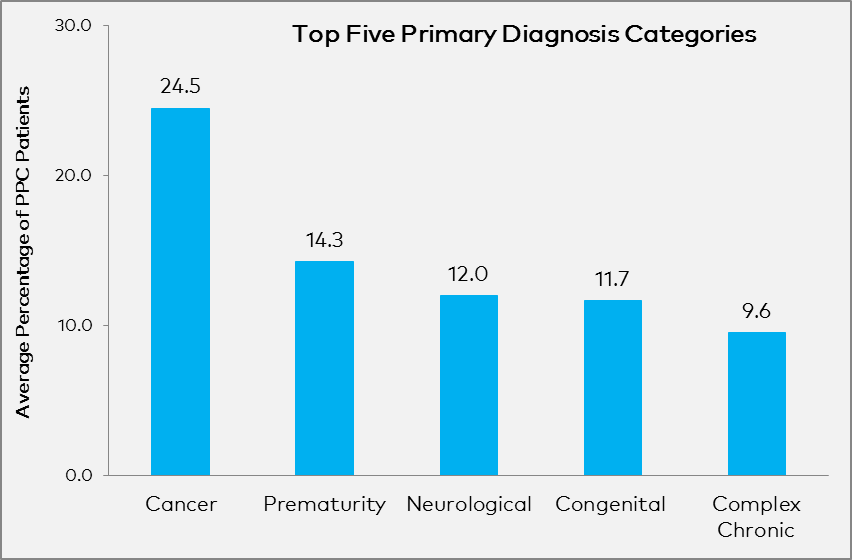
4. Pediatric palliative care programs treat patients with diverse primary diagnoses.
On average, nearly one-quarter of all pediatric palliative care patients had a primary diagnosis of cancer*. This was followed by prematurity (14.3%), a new diagnosis category that was added to the Registry survey this past year.
*These results differ from the 2011 article, Pediatric Palliative Care Patients: A Prospective Multicenter Cohort Study, which appeared in Pediatrics by Feudtner, et al. That study covered 515 patients seen by 6 academic hospital pediatric palliative care programs in the United States and Canada during 3 months in 2008. The study used different diagnostic categories and the study reported all diagnoses for patients (55% had more than one principal diagnosis). You can find more information on the 2011 pediatric palliative care study here:
Feudtner, et al. Pediatric Palliative Care Patients: A Prospective Multicenter Cohort Study. Pediatrics. 2011:127(6). https://www.ncbi.nlm.nih.gov/pubmed/21555495
5. Pediatric palliative care programs receive referrals from throughout the hospital, but the majority come from the ICU.
More than half of all pediatric palliative care patients are referred from the ICU. Only 21% of participating programs have standardized screening criteria to identify pediatric patients with palliative care needs in their hospitals.
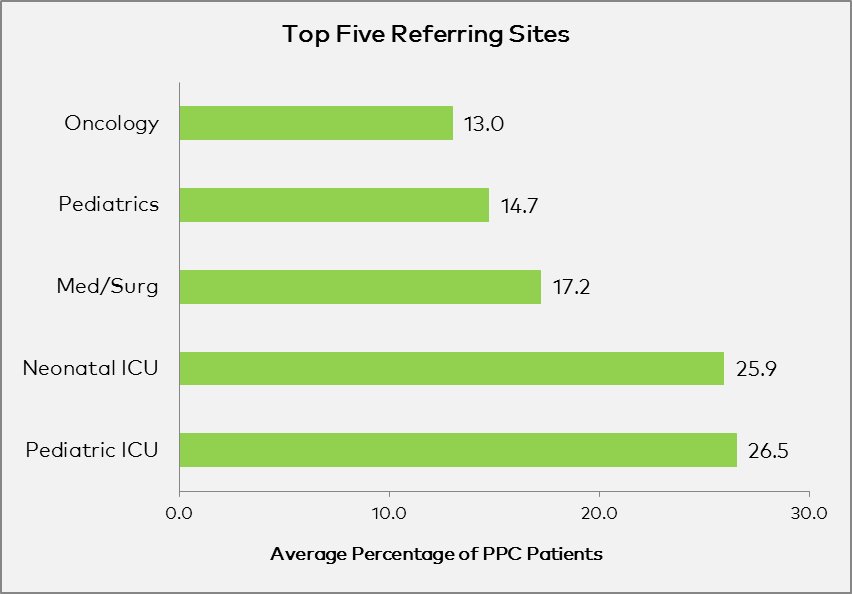
More than half of all pediatric palliative care patients are referred from the ICU.
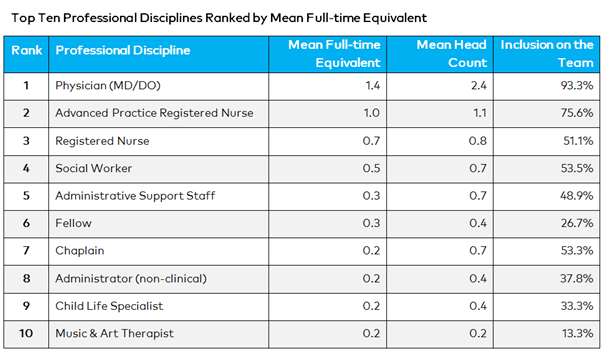
6. Pediatric palliative care programs report a variety of staffing models.
On average, pediatric palliative care programs consisted of almost nine staff members, representing just over five full-time equivalents (FTE). Staffing levels were related to the size of the hospital; for pediatric palliative care programs at hospitals with less than 250 pediatric beds/bassinets, the total FTE was 3.5 compared with 6.9 for hospitals with over 250.
The table below shows the top ten professional disciplines for pediatric palliative care programs in terms of full-time equivalency (the portion of time that a team member dedicates to the palliative care service). Physicians were the most frequent title reported (93.3% of programs reported having a physician included in the team) and had both the highest head count and FTE of all disciplines.
7. Most pediatric palliative care teams include staff with board certification in hospice and palliative medicine.
The majority (87%) of pediatric palliative care programs reported having at least one team member certified in palliative care or palliative medicine on their staff. Moreover, half of pediatric palliative care programs had a physician certified by the American Board of Medical Specialties (ABMS) in hospice and palliative medicine or an advanced practice registered nurse (APRN) certified in hospice and palliative care on their team.
8. Pediatric palliative care patients go home after being discharged from the hospital.
Participating programs reported that 75% of their patients were discharged from the hospital, and of those, 85% went home. Of the patients sent home, 21% received home hospice services. Other discharge locations included skilled nursing facilities, inpatient or residential hospice, acute inpatient rehab, general hospital, and other or unknown locations.
As these findings demonstrate, pediatric palliative care programs can use the National Palliative Care Registry™ to measure progress and track operational capacity and reach. There is no cost to participate or to receive data reports, and CAPC membership is not required. Greater numbers of programs participating will provide sufficient numbers to enable detailed pediatric-specific reports, and will enable further evolution of the database over time to better address the needs of pediatric programs. If you haven’t already done so, please enter your 2016 pediatric palliative care program data!
Help us to continue building the national profile of pediatric palliative care by participating in the National Palliative Care Registry™ today!
Citations
-
Meier DE. Increased Access to Palliative Care and Hospice Services: Opportunities to Improve Value in Health Care. Milbank Q. 2011;89(3):343–80. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3214714/
-
May P, Normand C, Morrison RS. Economic impact of hospital inpatient palliative care consultation: review of current evidence and directions for future research. J Palliat Med. 2014;17(9):1054-1063. http://www.ncbi.nlm.nih.gov/pubmed/24984168
-
Rabow MW, O’Riordan DL, Pantilat SZ. A Statewide Survey of Adult and Pediatric Outpatient Palliative Care Services. J Palliat Med. 2014;17(12):1311-1316. http://www.ncbi.nlm.nih.gov/pubmed/25137356
-
Feudtner C, Womer J, Augustin R, Remke S, Wolfe J, Friebert S, Weissman D. Pediatric Palliative Care Programs in Children’s Hospitals: A Cross-sectional National Survey. Pediatrics. 2013 Dec;132(6):1063-70. http://www.ncbi.nlm.nih.gov/pubmed/24190689
-
Denney-Koelsch E, Black BP, Cote-Arsenault D, Wool C, Kim S, Kavanaugh K. A Survey of Perinatal Palliative Care Programs in the United States: Structure, Processes, and Outcomes. J Palliat Med. 2016. Oct;19(10):1080-1086. https://www.ncbi.nlm.nih.gov/pubmed/27559768
-
Children’s Hospital Association. https://www.childrenshospitals.org/About-Us/About-the-Association
For further discussion of pediatric palliative care programs and the National Palliative Care Registry™, please join us at CAPC National Seminar 2017and Pre-Seminar Boot Camp.

