Key 2024 Palliative Care Billing Updates Every Provider Should Know

Every summer and fall, the Centers for Medicare & Medicaid Services (CMS) undertakes the task of updating the physician fee schedule (PFS) for the upcoming year. While some years witness minor adjustments, other years, such as 2023, undergo more sweeping and fundamental changes. These annual updates aim to align reimbursement rates with the current market conditions, reflecting changes in health care costs, technologies, and services, thereby supporting the delivery of high-quality health care.
In this article, we will break down how payment is calculated within the fee-for-service medicine framework. Having this understanding is crucial when trying to comprehend the PFS in its entirety. Then we will discuss the changes for 2024 in the recently-released PFS. If you are an expert in RVUs, feel free to skip the next section and go directly to the 2024 PFS update!
How is Payment Calculated in the Fee-For-Service Model?
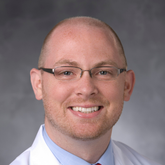
In the fee-for-service model, providers’ compensation is based on the specific services they provide. Each service, like a consultation or procedure, is assigned a distinct fee based on its relative value to other services. This value comparison is represented by what is known as the Relative Value Unit (RVU). Developed by CMS, this system aims to establish a fair means of assessing the value of clinical services (see Figure 1).
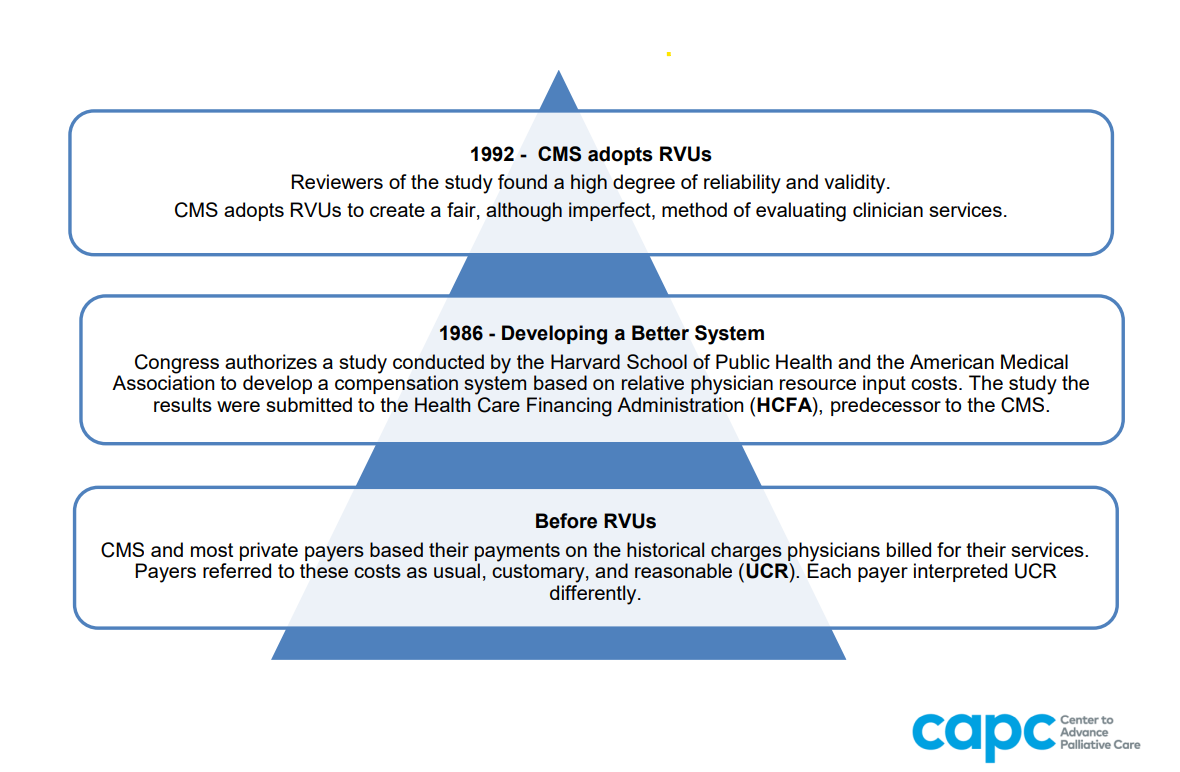
In health care, the RVU serves as a measure to quantify the value of medical services, taking into account factors such as a provider’s work, practice expenses, and malpractice insurance. RVUs play a crucial role in determining reimbursement rates in the fee-for-service model. The total RVUs assigned to a specific service contribute to the calculation of the payment that a clinician receives for that service. The model directly ties reimbursement to the volume and complexity of medical services provided. The total RVU is determined by the amount and complexity of work conducted (wRVU) and the expenses incurred by the provider in delivering that work (practice expense and malpractice expense). Considerations such as regional variations in the cost of practice and variations in malpractice costs for different specialties are factored into the total RVU calculation (see Figure 2). The Medicare Fee Schedule Lookup tool allows anyone to find the RVUs attached to a code and also lets you input your specific geographic locality to see the payment expected from fee-for-service Medicare.
After the total RVUs for a service are determined, this figure is multiplied by a CMS conversion factor to arrive at the payment for that service. The CMS conversion factor represents a dollar amount used in calculating payment for services within the Medicare Fee Schedule. It stands as a critical component in determining the reimbursement for various medical procedures and services covered by Medicare. This factor is subject to annual updates by CMS, accounting for changes in the cost of delivering health care services.
The 2024 Physician Fee Schedule
The recent update to the PFS for 2024 demonstrates a mix of positive developments and challenges for palliative care clinicians operating within the fee-for-service model.
Positive Developments
Notable wins include the extension of telehealth policies through December 31, 2024, especially the higher reimbursement rates for home-based telehealth services, and the unchanged 2024 Merit-Based Incentive Payment Systems (MIPS) performance threshold. Furthermore, the establishment of policies to bolster primary care, promote health equity, aid family caregivers, and expand access to behavioral health care all represent significant steps forward.
Noteworthy initiatives in the 2024 PFS include:
- Payment codes for time that clinicians spend training family caregivers of beneficiaries living with certain illnesses (utilizing codes 96202, 97550, 97551, and 97552, which will be finalized by January 1, 2024)
- New reimbursement codes for patient navigation services related to serious illnesses
- Payment for social determinants of health risk assessments (whether in person or via telehealth)
- Inclusion of qualified therapists and mental health counselors in Medicare billing starting January 1, 2024
G0136 Social Determinants of Health Risk Assessment
Specifically, the G0136 code pertains to the administration of a standardized Social Determinants of Health Risk Assessment tool. It evaluates an individual's social risk factors affecting the diagnosis and treatment of medical conditions, taking approximately 5-15 minutes with an associated wRVU of 0.18.
G0019 and G0022 Community Health Integration
G0019 and G0022 codes focus on Community Health Integration, introducing separate coding and payment for such services. These can be provided by trained auxiliary personnel (e.g., community health workers) under a qualified billing clinician's direction using ‘incident to’ billing rules. Monthly billing follows an initiating visit where social determinants of health needs are identified. G0019 (1.0 wRVU) covers 60 minutes of staff time per calendar month, and G0022 (0.7 wRVU) is reported for each additional 30 minutes.
G0023 and G0024 Principal Illness Navigation
Lastly, G0023 and G0024 codes relate to Principal Illness Navigation services provided by certified or trained auxiliary personnel under a clinician's direction, again using ‘incident to’ billing. This includes patient navigation, assisting patients with complex or high-risk conditions, and teaching patients self-advocacy skills. G0023 (1.0 wRVU) is reported for 60 minutes per calendar month, and G0024 (0.7 wRVU) is reported for each additional 30 minutes.
Add-On Code for Complex Patients G2211
G2211 is an additional code that complements office and outpatient services (99202–99215) and is intended for primary care and other specialties managing a single, serious, or complex condition consistently over an extended duration. CMS emphasizes the importance of the practitioner-patient longitudinal relationship.
It is designed for practitioners relying heavily on Evaluation and Management (E/M) services to be paid for their work. CMS asserts that the current valuation of office visit codes does not sufficiently capture the cost of managing the intricacies of specific visits over time. According to CMS, the values fail to consider the resource costs linked to primary care and the longitudinal care of complex patients. As defined, this add-on code certainly applies to visits performed as part of palliative care that is provided longitudinally (over time) in the office or other community settings.
Challenges
While these improvements are positive, the reduction in the conversion factor from $33.06 in 2023 to $32.74 in 2024 presents a considerable challenge for fee-for-service providers. According to Anders Gilberg, senior vice president of government affairs at the Medical Group Management Association (MGMA), this reduction in the 2024 Medicare conversion factor further widens the gap between physician practice expenses and reimbursement rates, posing potential financial strains for health care practices. As the cost of doing business increases due to inflation (salaries, supplies, etc.), this decrease in reimbursement will cause challenges to be sure.
The takeaway for palliative care teams? Get to know the new billing possibilities in the 2024 PFS, and make sure that you are optimizing your billing practices to reflect the complicated work that you do.
The takeaway for palliative care teams? Get to know the new billing possibilities in the 2024 PFS, and make sure that you are optimizing your billing practices to reflect the complicated work that you do.
CAPC Resources for Understanding the 2024 Medicare Physician Fee Schedule
The Center to Advance Palliative Care (CAPC) is committed to providing palliative care teams with detailed guidance on billing every year when the new PFS is published. Additionally, CAPC hosts Virtual Office Hours and webinars on best practices in billing, and a host of additional resources to assist health care professionals in navigating the evolving landscape of health care billing, reimbursement, and delivery.
- Register for the 2024 Billing and Coding for Palliative Care: Navigating New Opportunities webinar, presented by Christopher Jones, MD, MBA, and Phillip Rodgers, MD, FAAHPM, February 15, 2024 at 1:30 pm ET.
- Explore our comprehensive Optimizing Billing Practices toolkit, updated to reflect the 2024 changes to the PFS.
- For a closer look at RVUs, read our blog, Everything You Always Wanted to Know about RVUs But Were Afraid to Ask, by Lynn Spragens, MBA, and Allison Silvers, MBA.

Be the first to read articles from the field (and beyond), access new resources, and register for upcoming events.
Clinical review by Andrew Esch, MD, MBA.