Introducing a New, Non-Residential, Community-Based HPM Fellowship

Dr. Brandy Drake received her training and has worked as an emergency medicine physician in the small mountain town of Glenwood Springs, Colorado. Throughout this time, especially over the past 10 years, she’s became increasingly aware of the need for palliative care in the emergency department (ED), hospital as a whole, and community, as more frail and elderly people living with serious illness have turned to the ED in crisis.
A Desire to Develop Palliative Care Skills
A few years ago, Dr. Drake watched with interest as her colleague, a physician assistant, enrolled in the Master of Science in Palliative Care (MSPC) at the University of Colorado Anschutz Medical Campus (CU Anschutz). His goal was to integrate palliative care in the radiation oncology clinic where he worked, but also in the community more broadly. As he shared what he was learning, and Dr. Drake saw what these new skills brought to their patients, she felt like she also needed to pursue this course of study.
The following year, Dr. Drake, along with another colleague, a nurse practitioner, both enrolled in the MSPC program and simultaneously started a new consult service within their hospital. While Dr. Drake’s ultimate goal is to become board certified in Hospice and Palliative Medicine (HPM), leaving her community and job, and uprooting her family is not a possibility – even if she were accepted into one of the limited number of U.S. HPM fellowship slots.
This is a common story that plays out across the country, which CU Anschutz sought out to fix by developing, and now offering, a novel solution.
An Alternative Pathway for Mid-Career Physicians
There is a serious shortage of palliative care specialists in all disciplines in health care, with the physician pipeline presenting a particularly difficult problem. Currently, there are only 360+ physicians training each year to be HPM specialists, and we need several times that number in order to meet the demand that our aging population will require.
In response to this crisis, the University of Colorado School of Medicine is now offering a first-in-the-nation non-residential HPM fellowship. This means that our mid-career palliative medicine candidates do not have to move away from home, nor abandon their work and family responsibilities, in order to receive training that prepares them to sit for board certification. This could not have happened without substantial support from my colleagues in Colorado, as well as significant encouragement and expertise from the American Council on Graduate Medical Education (ACGME), the American Board of Internal Medicine (ABIM), and the American Board of Family Medicine (ABFM), and many others. We are proud to have developed this fellowship program, to help bridge a need for those mid-career physicians who would have otherwise been unable to become board certified in palliative medicine due to life circumstances.
We are proud to have developed this [non-residential] fellowship program, to help bridge a need for those mid-career physicians who would have otherwise been unable to become board certified in palliative medicine due to life circumstances.
Community-Based Fellowship Training: Stay and Train in Your Community
We have found that physicians are often drawn to the field of palliative care in mid-career, once they’ve witnessed how their patients and family caregivers could benefit. However, it is often difficult or even impossible to leave their families, communities, and medical practices in order to relocate for subspecialty palliative medicine fellowship training.
To solve for that, beginning in the summer of 2020, 6 mid-career physicians will begin training in the new Community Based Hospice and Palliative Medicine Fellowship (CB-HPM) demonstration project. And lucky for us, Dr. Drake will be one of them.
How the Program Will Work
Eligibility for board certification requires a set of qualifications for practitioners and allows for oversight by peers who can ensure high standards of care. In order to ensure that our program was accredited for board certification, the team at CU Anschutz worked with Eric Holmboe, MD, of the Accreditation Council for Graduate Medical Education (ACGME) to develop a program of online asynchronous study and work review, paired with biweekly video conferences for oral case presentation and discussion. Physicians who are accepted and enrolled as students in the MSPC program may apply for the Community Based-Hospice and Palliative Medicine Fellowship Seminars. The Master of Science in Palliative Care (MSPC) provides in-depth interprofessional palliative care didactics.
As part of HPM seminars, physician fellows will have clinical experiences in their own community, such as consulting on palliative care patients and submitting their consultation assessments and recommendations on-line. They will also present patients through video conferencing to the HPM faculty here at CU Anschutz for direct supervision and feedback. Thus oversight, feedback, and role modeling from expert faculty will occur, just as it does in the traditional fellowship. Other seminar activities include role-play, journal clubs, discussion of assigned readings, and video demonstration of assessment techniques. Through a secure online palliative medicine clinical portfolio, fellows will submit their consultation and clinical experience, the written consultations themselves, and number and type of exposures to the key elements of the required competencies (new ACGME Milestones). Faculty evaluation, feedback, and response to feedback will be documented, along with faculty assessment of the level of achievement of the required milestones/key competencies. Fellows will concurrently complete the MSPC degree, which includes a capstone palliative care quality improvement project in their home setting. In this manner, fellows will meet all HPM fellowship and board eligibility requirements, over a two-year period.
Comparison Chart of CU Anchutz Programs
| Interprofessional Palliative Care Certificate (IIPC) - Community Specialist | Master of Science in Palliative Care (MSPC) - Community Specialist | Non-Residential Community-Based HPM Fellowship (CB-HPM) | |
|---|---|---|---|
| Length of Program | 2 semesters (9 months) | 6 semesters of continuous study (2 years) |
2 Years* *Fellow is board eligible when both the MSPC and CB-HPM Fellowship are successfully completed |
| Who it is for? | Nurses; Nurse Practitioners; Physicians; Physician Assistants; Pharmacists; Spiritual Care providers; Social Workers; Psychologists; Other (Child Life Specialists, Grief Counselors, Community Navigators, etc.) | Nurses; Nurse Practitioners; Physicians; Physician Assistants; Pharmacists; Spiritual Care providers; Social Workers; Psychologists | Medical Doctors (MD); Doctors of Osteopathic Medicine (DO) |
A History of Creative Solutions for Mid-Career Providers
As innovators in medical education the CU Anschutz faculty have a history of palliative care education.
Masters of Science in Palliative Care
We started the country’s first Master of Science in Palliative Care (MSPC) program in 2016, an interprofessional course of study which has enabled 66 physicians, nurses, physician assistants, advanced practice providers, social workers, spiritual care providers, pharmacists, psychologists, and others to advance their knowledge and skills through a primarily online format.
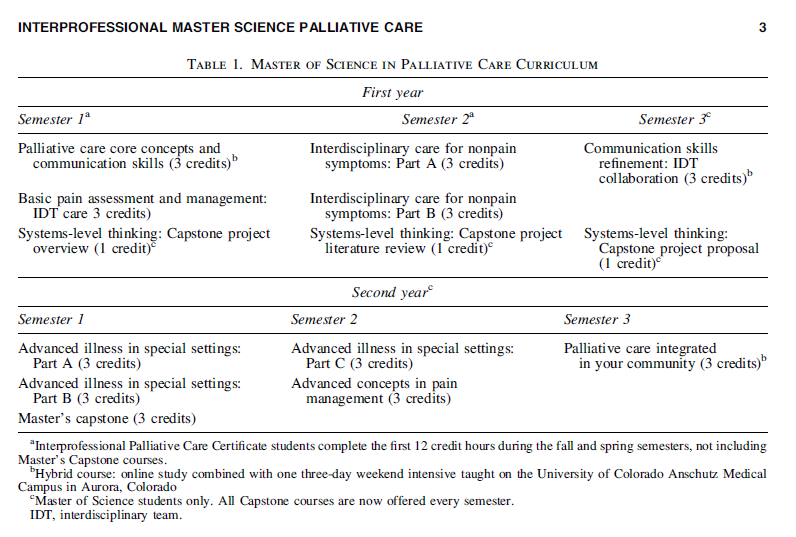
Once enrolled, participants attend 3 on-campus weekend intensive sessions to focus on communication training. The first 4 courses (12 credits over a 9-month period, including 1 on-campus weekend session) comprise the interprofessional palliative care certificate (IPCC) program, focusing on palliative care core concepts and principles, pain and non-pain symptoms, and psycho-sociocultural-spiritual-ethics components. Students in their second year apply palliative care principles in different disease processes, locations of care, and populations, refine communication skills, and complete a capstone project in their community, earning a MSPC.
Below is an overview of the MSPC program, as published in the Journal of Palliative Medicine.
The Role of Palliative Care Community Specialists
The existing MSPC program has been ideal for mid-career clinicians, as it allows them to train as “palliative care (PC) community specialists”, while remaining in their home, community, and practice. Community specialists provide high quality palliative consultation and care to patients and families in their own communities, giving patients and families the option to be cared for near their homes, outside of an academic tertiary medical center. PC community specialists bridge a network of services to better support the needs of patients and their families, across the continuum of serious illness.
Revisiting the CB-HPM Fellowship
The new CB-HPM Fellowship incorporates the Master of Science in Palliative Care (MSPC) foundation, and then supports physicians with mentored clinical experience paired with assessment and feedback on the required HPM competencies, to become board-eligible for board certification in HPM.
This program holds great promise as an alternative pathway for mid-career physicians to enter the field of HPM.
This fellowship program holds great promise as an alternative pathway for mid-career physicians to enter the field of HPM. This model could also be used to support the development of specialists in other areas, like geriatrics or addiction medicine, where career development is necessary to provide the best care for patients. Additionally, this program overcomes the barriers to such training posed by the traditional requirement to forgo professional and personal responsibilities in mid-life to relocate to another community for a residential fellowship program.
Other medical schools are also coming up with creative solutions to the workforce shortage, such as the University of Pennsylvania, explained in Dr. Laura Dingfield’s 2019 blog post.
In Conclusion
With the new non-residential fellowship program, physicians now have the ability to complete an HPM Fellowship, become board-eligible, and bring much needed specialist-level palliative care to their communities. And all other disciplines are able to become PC community specialists through the other training programs: Master of Science in Palliative Care (MSPC) and Interprofessional Palliative Care Certificate (IPCC).
For more information about our programs, visit our website or email me directly at [email protected].
