Five Key Insights on Hospital Palliative Care Programs
This year, 54 pediatric and 425 adult or mixed inpatient palliative care programs submitted data on their program operations to the National Palliative Care Registry™. While not representative of all hospitals with palliative care in the United States, these programs are composed of hospitals of all sizes, ownership, teaching status, and are located across the US. The insight gleaned from the Registry can guide our understanding of palliative care program operations in an effort to strengthen program development strategies and standards.
Here are five key findings on inpatient palliative care programs:
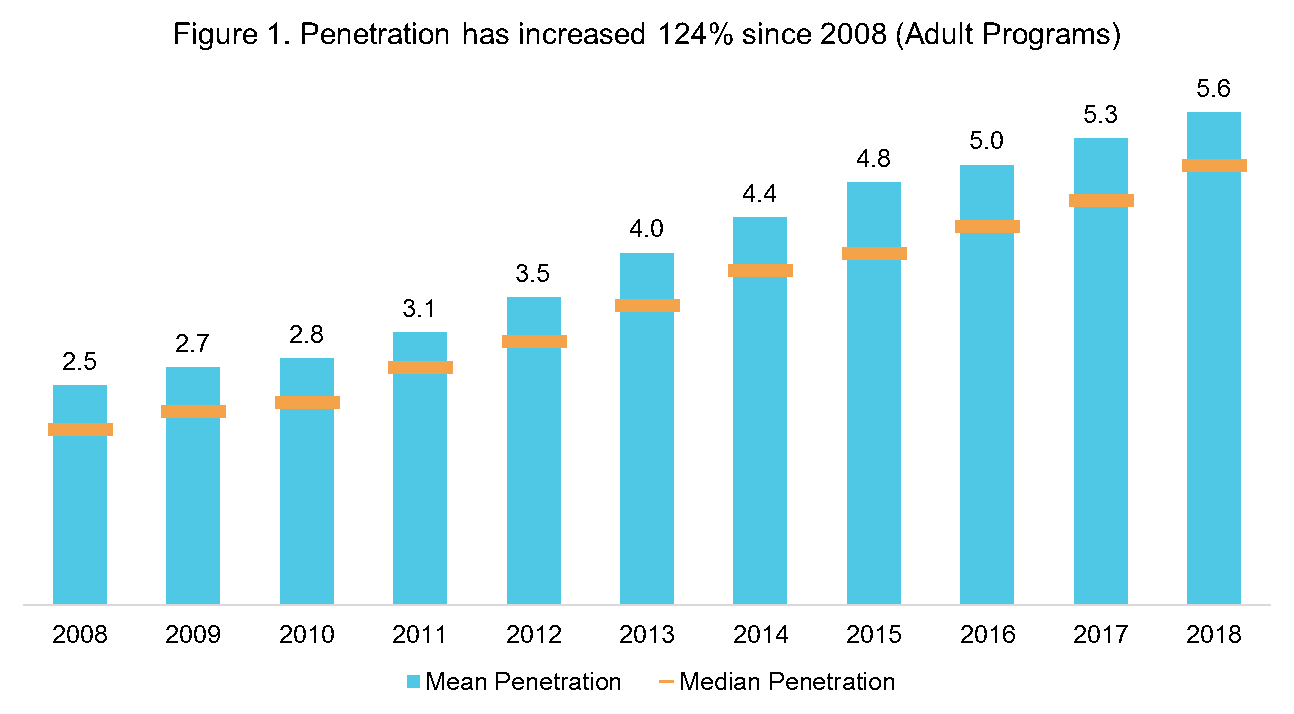
1. Each year, inpatient palliative care programs reach more patients in need.
In 2008, inpatient programs were providing initial palliative care consults to an average of 2.5% of annual hospital admissions (penetration), or for every 40 people admitted to the hospital annually, one was receiving an initial palliative care consult. In 2019, palliative care programs reported providing consults to 5.6% of annual hospital admissions. This means that for every 18 people admitted to the hospital annually, one received an initial palliative care consult.
Many factors can impact palliative care penetration rates, including the size of the hospital, the age and staffing level of the palliative care program, and the hospital’s teaching status. Pediatric palliative care programs have lower penetration rates with an average of 3.1%. Growth in palliative care penetration is a measure of how well we are reaching patients in need.
Growth in palliative care penetration is a measure of how well we are reaching patients in need.
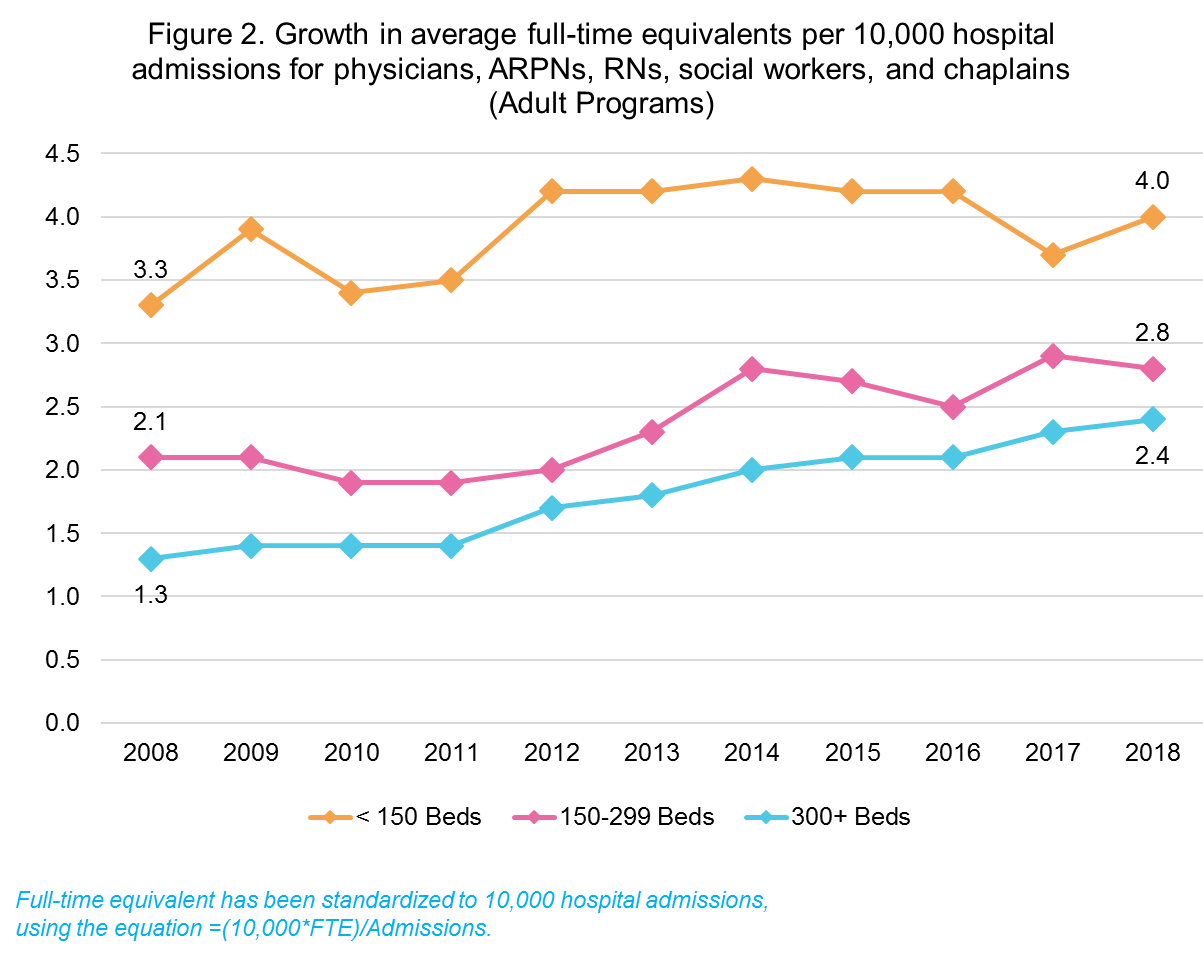
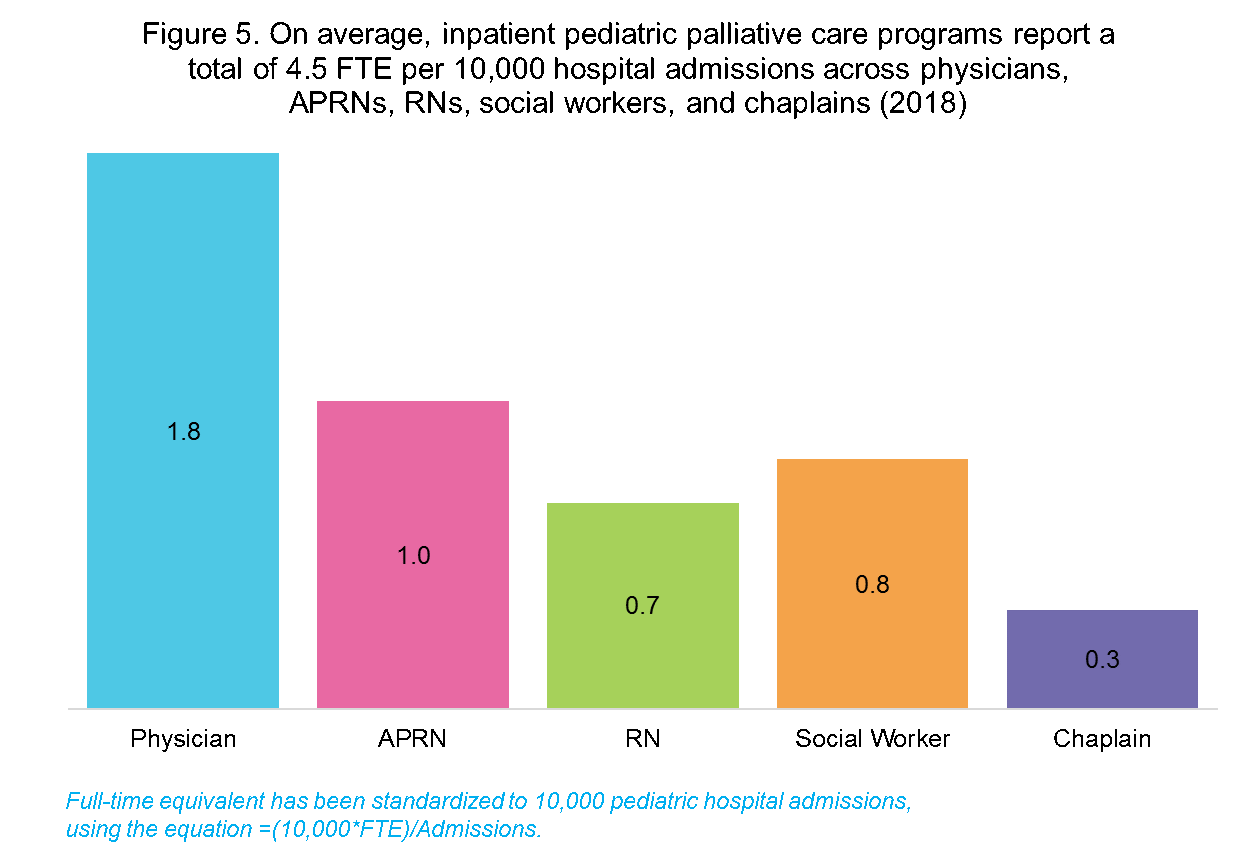
2. Inpatient palliative care programs are not equitably staffed.
While physicians, advanced practice registered nurses and registered nurses, social workers, and chaplains are the most commonly reported disciplines by palliative care teams, only 37% of pediatric programs and 41% of adult programs reported staff from each of these critical disciplines. Staffing levels represented in full-time equivalents per 10,000 hospital admissions show significant variation across hospital size, and in longitudinal analyses, the growth in FTEs has been the greatest in larger hospitals. Further, programs with a larger number of FTE per 10,000 hospital admissions are more likely to hit a higher penetration and reach more patients in need. (Check out CAPC's toolkit, Building and Supporting Effective Palliative Care Teams, which includes resources on staffing.)
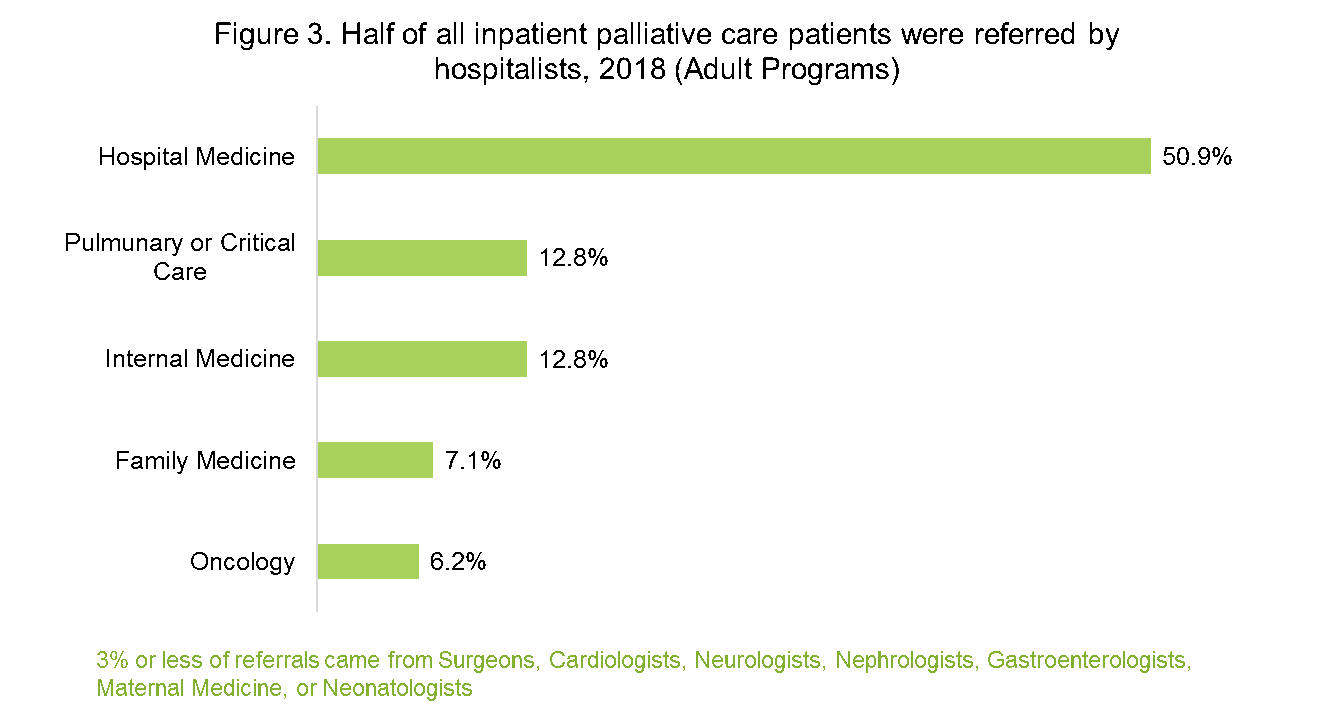
3. Hospitalists perform an essential role in identifying palliative care needs and referring to palliative care programs.
On average, half of all adult inpatient palliative care patients were referred to palliative care by hospitalists, more than triple the percentage of referrals from any other specialty. Most hospitalized patients are treated by hospitalists during their admission. Ensuring that hospitalists have the appropriate skills in communication, pain and symptom management, and caregiver support will help ensure that all patient’s seen by hospitalists will benefit from skilled communication and symptom management, and that specialist palliative care teams serve as consultants for the most complex patients. (Check out CAPC’s Hospital Medicine learning pathway and recent blog post, 5 Ways to Improve Hospitalist-Palliative Care Collaboration.)
4. Many inpatient programs are not yet meeting national guidelines on the structure and processes of care.
The fourth edition of the National Consensus Project (NCP) Guidelines for Quality Palliative Care provides recommendations for palliative care programs across eight domains, including Domain 1 on structure and processes of care. Responses in the Registry show that fewer than half of adult programs ensure 24/7 program availability to patients and families and 46% do not have access to chaplains or other spiritual support. Over 80% have at least one team member board-certified in palliative care.
Figure 4. Percent of programs meeting National Consensus Project Guidelines (2018)
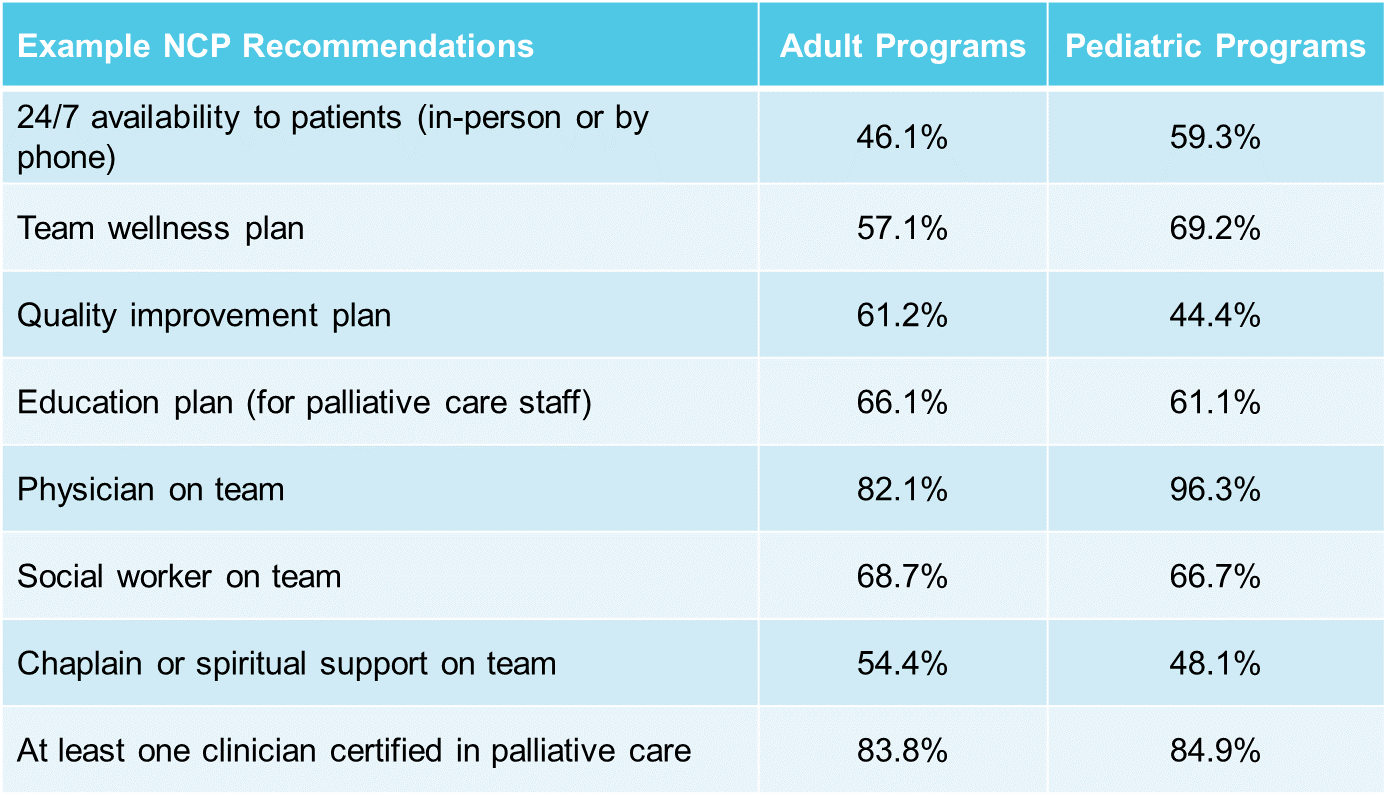
5. Pediatric palliative care programs are different from adult programs.
From staffing models to program features to consult volume, pediatric palliative care programs operate differently. Pediatric palliative care programs provide more follow-up visits per consult than adult programs (4.3 versus 1.8) and are more likely to report having physicians, child life specialists, and palliative care fellows on their team. Pediatric programs also reported providing consults for end-of-life or hospice referral at a significantly lower rate than adult programs. Pediatric palliative care programs were more likely to receive funding from philanthropy than their adult counterparts.
__________________________________________________________________________________________________
Leveraging Data to Make Change
National comparative data from the Registry helps programs compared themselves to peers, and provides data making the case for improvements in staffing levels, training, quality standards, and penetration. To learn more about how the Registry has supported the growth and sustainability of palliative care programs, read our September 2019 Article in the Journal of Palliative Medicine.
For more trends and insights from the Registry, listen to the recorded August 2019 webinar, Latest Trends and Insights from the National Palliative Care Registry™, and download the corresponding slides (open to members and non-members).
A Note about the Future of the National Palliative Care Registry™
In 2020, the National Palliative Care Registry™ will be relocating to a new home in the Palliative Care Quality Collaborative (PCQC). Through PCQC, structure and process data, as well as comparative reports and key findings on program operations will still be collected and available for free to all participating palliative care programs. PCQC will also enable teams to submit patient-level data to drive quality improvement and quality measurement initiatives. Patient-level data submission will require an annual fee.
PCQC will launch during the second quarter of 2020 and will be open to all palliative care programs across the continuum. PCQC is a collaboration of five national palliative care organizations: American Academy of Hospice and Palliative Medicine (AAHPM), Center to Advance Palliative Care (CAPC), Global Palliative Care Quality Alliance (GPCQA), National Palliative Care Research Center (NPCRC), and Palliative Care Quality Network (PCQN).
For any questions about the Registry or PCQC, please contact the CAPC Research & Analytics Department at [email protected].
