Independence through Interdependence: Washington Rural Palliative Care Initiative
One in five Americans live in rural settings. Compared to urban populations, rural residents have less access to specialized healthcare services, including palliative care (PC). Limitations on access to palliative care in rural settings include a lack of clinical training, limited healthcare resources, limited caregiver availability, high staff turnover, and administrative resistance to funding dedicated PC staff given low patient volumes. Rural residents are also less likely to have employer-sponsored health insurance coverage, and those who are impoverished often do not have Medicaid coverage. Given that rural populations are more likely to have chronic medical conditions and/or physical disability than urban Americans, the lack of access to PC services creates significant inequities for these communities.
The Washington Rural Palliative Care Initiative (WRPCI) was founded in 2016 as a public-private partnership led by the State Department of Health's Office of Rural Health with over 20 partner organizations, largely grant-funded by both private and public payors. Its primary objective is to assist rural health systems and communities integrate palliative care across various settings to better serve people with serious illness. A community engagement strategy assembled diverse strategic partners in each community for an asset/ gap analysis and to develop an individualized action plan. A Learning Action Network creates networking and problem-solving opportunities among participating communities. All communities participate in online clinical case consultations and office hours with an interdisciplinary PC team, didactic sessions, and individualized team mentoring.
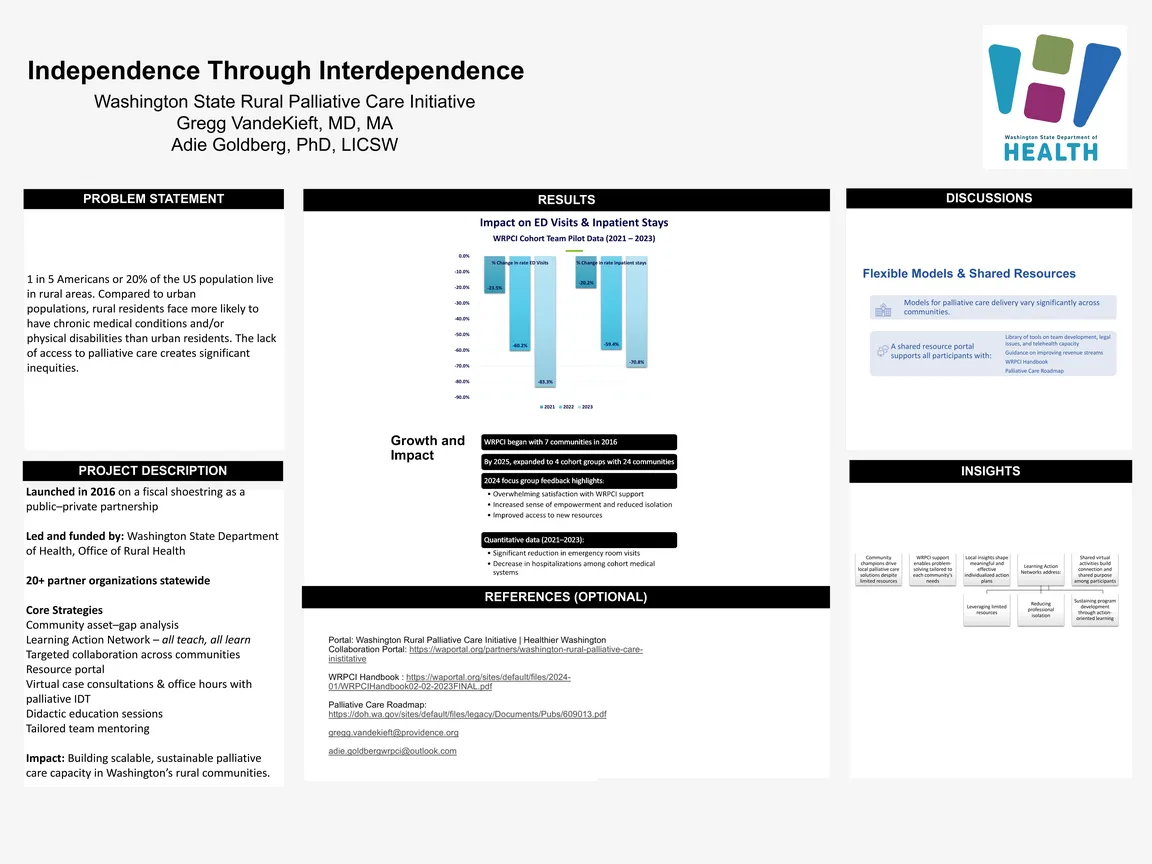
The original cohort of seven communities in 2016 has expanded to four cohorts with 24 communities in 2025. Qualitative data from participants (focus groups, 2024) reflected overwhelming satisfaction with the support provided by the WRPCI, noting a sense of empowerment, decreased isolation, and increased ability to access new resources. Quantitative data analysis of participating cohorts from 2021-2023 demonstrated significant reduction of emergency department visits and hospitalizations. Models of palliative care delivery vary significantly across communities. A shared resource portal contains a library providing information on team development, assessing community telehealth capacity, legal issues, opportunities to improve revenue streams, and other topics, as well as the WRPCI Handbook and a Palliative Care Road Map.
Community champions carry the message that local problem-solving, supported by the WRPCI, enables the delivery of palliative care in their community despite limited resources. While the core WRPCI interdisciplinary team provides access to specialized PC knowledge and skills, each community's understanding of local organizations, resources, and community culture brings depth and meaning to the individualized action plans. The Learning Action Network model facilitates shared learning among participating communities on topics such as leveraging limited local resources, reducing professional isolation, creating action-oriented learning models, and sustainable program development. Shared virtual activities have promoted a sense of community among the participating communities.
Authors
- Gregg VandeKieft, MD, MA, (Providence Swedish)
- Adrienne Goldberg, PhD, LICSW, M.Ed. (Washington State Department of Health, Office of Rural Health)