Improving Early Access to Palliative Care
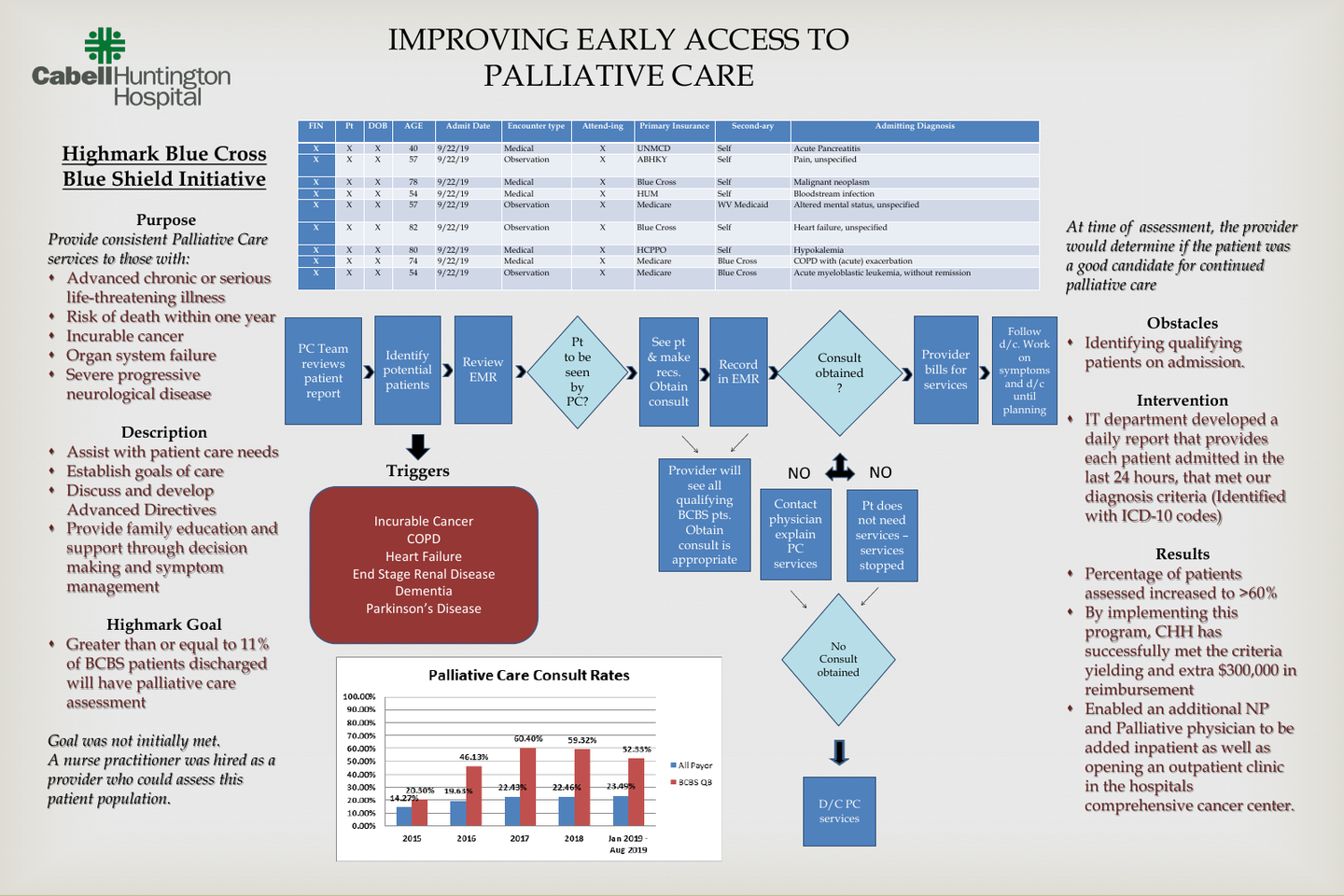
Highmark Blue Cross Blue Shield established a program in 2016 to continue and support focus on improving quality of life for patients with advanced serious or complex issues. This initiative listed specific criteria for patients including cancer diagnosis, congestive heart failure, chronic pulmonary disease, as well as dementia. This patient population was to be assessed by a palliative care provider during the hospital admission to address symptom management, goals of care discussions, and disease trajectories. Initially, the goal for this initiative was 14% of patients with a history of advanced or chronic illness be assessed by a palliative care provider. The initial state of palliative care involvement, of these patients, was 11%.
In 2015, Cabell Huntington Hospital was not meeting this requirement. Therefore, a nurse practitioner was hired on as a palliative care provider. The provider at that point would be able to assess patients to ensure symptoms were well controlled, as well addressing the patient’s goals of care, and understanding the disease process. If the provider felt a referral to the palliative care team was appropriate, one would be obtained from the primary admitting physician. Once this consultation was in place, the provider could then assist with code status orders, symptom management medication orders, and referrals to hospice, as well as other outside resources.
One of the largest obstacles was identifying these patients on admission so that the patient could be assessed by a palliative care provider. The IT department developed a daily report that provides each patient admitted to the hospital in the last 24 hours. This report contains patient demographics as well as the chronic or terminal diagnosis of the patient, that has been listed in the nursing history. The palliative team reviews this list daily to determine if the patient meets the criteria to be evaluated. This report has increased access to these patients earlier in the disease process as well as increased overall referrals to the palliative care team.
In 2015 when the program was put into place, the percentage of Blue Cross patients with chronic or terminal illness that was being assessed by a palliative care provider was at 11%. Once the palliative care report was formulated, the percentage of patients with a chronic or terminal illness increased to 60.4%. This increase has remained consistent over the last few years. This has increased overall referrals by more than 20%, allowing an outpatient clinic to be open within the hospitals comprehensive cancer center and allowing for an additional NP and physician to the inpatient team.
By implementing this program established by Blue Cross Blue Shield, Cabell Huntington Hospital has successfully met the criteria yielding an extra $300,000 in reimbursement. This initiative has also been successful in facilitating earlier referrals, more education on disease processes, completion of Advanced Directives, and overall assessments of symptom management and earlier referrals to community resources. Cabell Huntington Hospital continues to strive to provide early intervention, support, and education in palliative care appropriate patients.
Author
Shannon A. Runnels, APRN, FNP-C
Cabell Huntington Hospital
1340 Hal Greer Blvd
Huntington, WV 25701
(304) 399-6874