Improving Access to Community Palliative Care within an ACO: Lessons Learned
Background: Community-based palliative care enhances the value of healthcare for persons with serious illness, yet access to services remains dependent on clinician referrals. Given their value-based focus and population health approach, Accountable Care Organizations (ACOs) provide a potential opportunity for proactive and consistent palliative care referral for seriously-ill patients. In this report, we describe a collaboration between an ACO and a palliative care program to use semi-automated screening to improve efficient and systematic identification of seriously-ill patients in order to increase access to palliative care services.
Aims: Within a Medicare Next Generation ACO (1) To develop a risk scoring screening tool to identify seriously-ill patients who may benefit from community-based palliative care services, and (2) To assess referrals to community-based palliative care using triggered electronic health record (EHR) alerts combined with use of the screening tool.
Methods: An ACO and a community-based palliative care program collaborated to create an EHR triggered alert to generate weekly reports of ACO patients who had a non-elective inpatient admission at one of three hospitals in central North Carolina and lived within the area covered by community-based palliative care program. They also created a risk scoring screening tool based on current evidence for identifying patients with palliative care needs that assessed seven domains: (1) age, (2) presence of specific life-limiting illnesses, (3) functional status, (4) absence of advance care planning, (5) poor psychosocial support, (6) high hospital/emergency department utilization, and (7) uncontrolled symptoms. Chart reviews were used to apply this risk score to all patients identified by the EHR trigger. Patients with scores < 3 were categorized as unlikely to benefit, between 3 and 5 categorized as potentially benefitting and > 5 were categorized as likely to benefit.
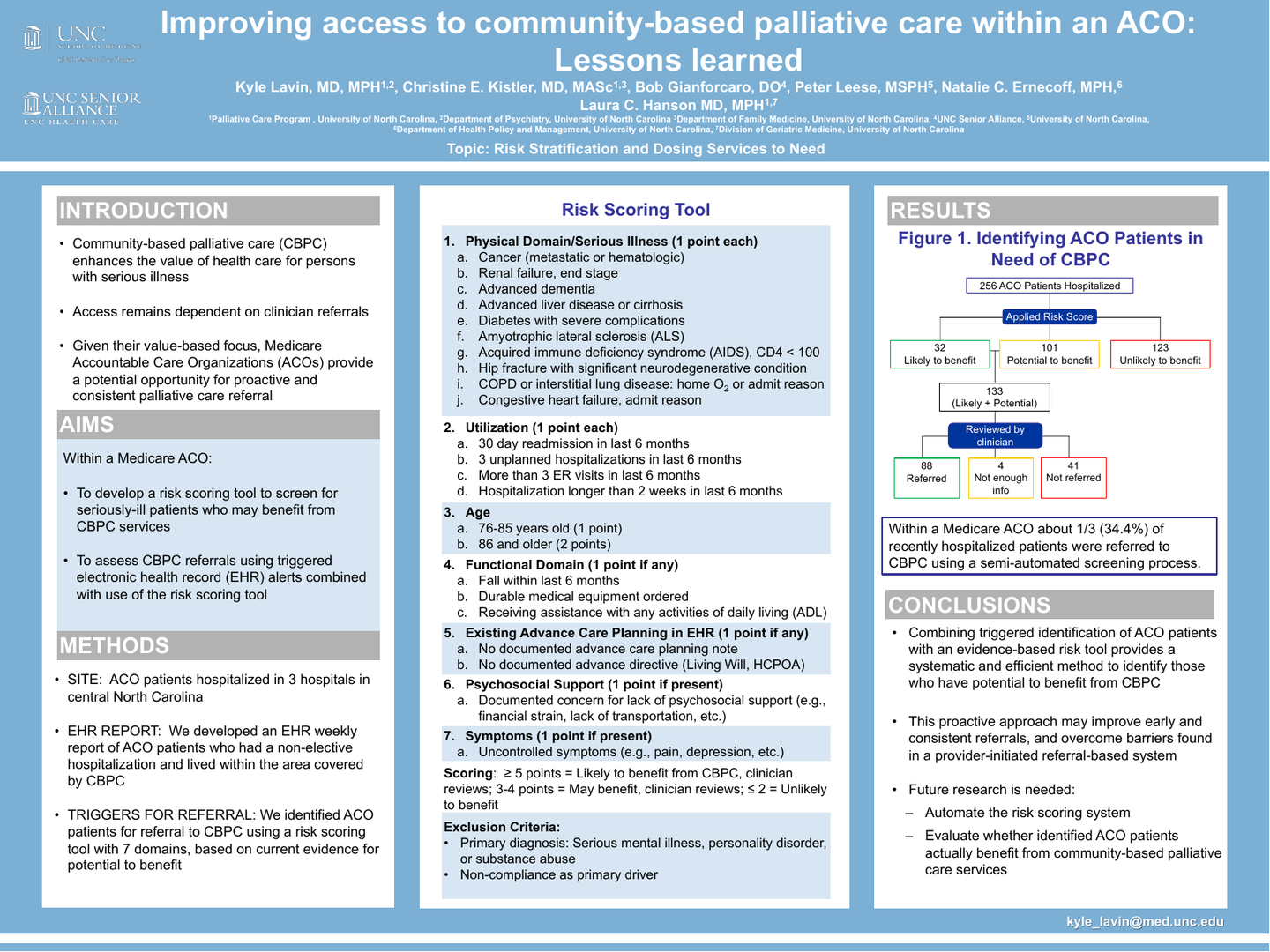
Results: Over a 10-week period the EHR trigger identified 256 ACO patients who were hospitalized. Based on the risk scoring tool, 32 were categorized as likely to benefit from palliative care, 101 as potentially benefitting, and 123 as unlikely to benefit. A palliative care specialist further reviewed the 133 patients scored as likely or potentially benefitting from palliative care and based on clinical expertise recommended 88 be referred for palliative care, 41 not be referred, and that 4 lacked sufficient information to make a determination. For patients recommended for referral the primary physician was contacted by the palliative care specialist via standardized EHR messaging to initiate the referral process.
Conclusions: Within a Medicare ACO over 1/3 (34.4%) of recently hospitalized patients would likely benefit from palliative care and were referred using a semi-automated screening process. Combining triggered identification of patients with an evidence-based risk screening tool provides a systematic and efficient method to identify patients with potential to benefit from palliative care. This proactive approach may improve early and consistent referrals and overcome barriers found in a provider-initiated referral-based system. Future work is needed to automate this risk scoring system and to evaluate whether identified patients actually benefit from community-based palliative care services.
Author
Kyle Lavin, MD
MD, MPH
UNC Chapel Hill School of Medicine
101 Manning Dr
Chapel Hill, NC, 27514