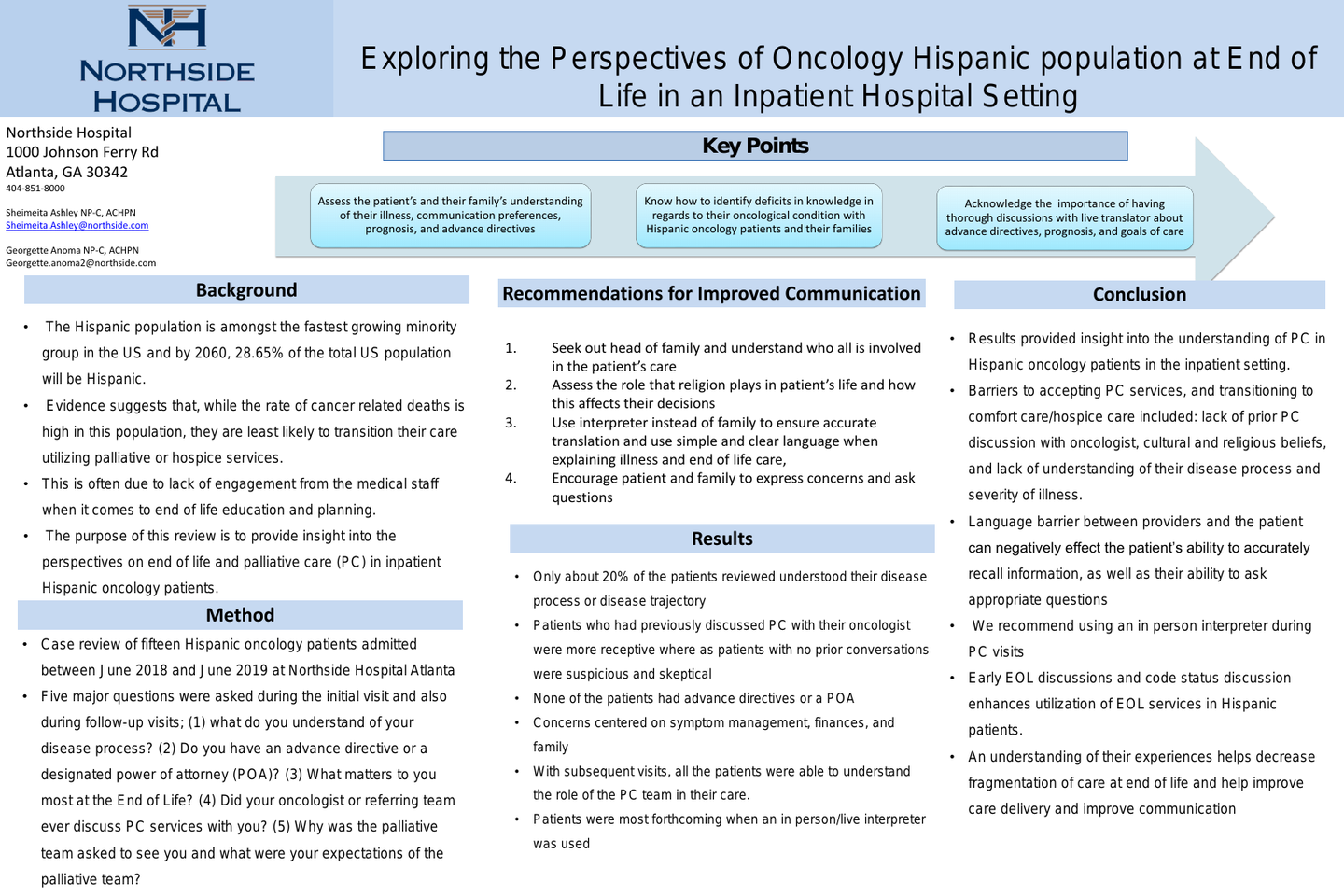
Exploring the Perspectives of Oncology Hispanic Population at End-of-Life in an Inpatient Hospital Setting
Background
The Hispanic population is amongst the fastest growing minority group in the United States. By the year 2060, 28.65% of the total US population will be Hispanic. As this population grows, they are likely to experience life limiting illnesses along with health disparities due to language barriers, health illiteracy, and lack of resources. Such disparities have a significant impact on overall mortality rates in this demographic group. Cancer is the leading cause of death among Hispanics, accounting for 21% of deaths. Evidence suggests that, while the rate of cancer related deaths is high in this population, they are least likely to transition their care utilizing palliative or hospice services. This is often due to lack of engagement from the medical staff when it comes to end of life education and planning. The purpose of this review is to provide insight into the perspectives on palliative care (PC) in inpatient Hispanic oncology patients.
Method
A case review of fifteen oncology patients admitted between June 2018 and June 2019 was completed. All of these patients were of Hispanic descent. Five major questions were asked during the initial visit and also during follow-up visits; (1) what do you understand of your disease process? (2) Do you have an advance directive or a designated power of attorney (POA)? (3) What matters to you most at the End of Life? (4) Did your oncologist or referring team ever discuss PC services with you? (5) Why was the palliative asked to see you and what were your expectations of the palliative team?
Results
Of all the patients reviewed, > 50% had advanced disease and poor functional status. Only about 20% of the patients reviewed understood their disease process and were able discuss the trajectory of their disease. For those patients who had previously discussed PC with their oncologist, they were more open to having us participate in their care. For those who had not previously discussed PC, they reacted with suspicion and skepticism. None of the patients had advance directives or a POA. What mattered most to the participants centered on symptom control, family, finances, and spirituality. With subsequent visits, all the patients were able to understand the role of the PC team in their care. When a certified interpreter in person/live interpreter was used, the patients was more forthcoming with information.
Conclusion
The results of this study provided insight into the understanding of PC in Hispanic oncology patients in the inpatient setting. Barriers to accepting PC services, and transitioning to comfort care/hospice care included: lack of prior PC discussion with oncologist, cultural and religious beliefs, and lack of understanding of their disease process and severity of illness. It is recommended that an in person interpreter be used when palliative care meets with this population. Achieving a better understanding of their experiences with the hope of decreasing fragmentation of care at end of life can help improve care delivery and improve communication between this population and providers.
Author
Sheimeita Ashley, MSN, NP-C, ACHPN
Palliative Medicine Nurse Practitioner
Northside Hospital
1000 Johnson Ferry Road
Atlanta, GA 30342
(404) 843-8965