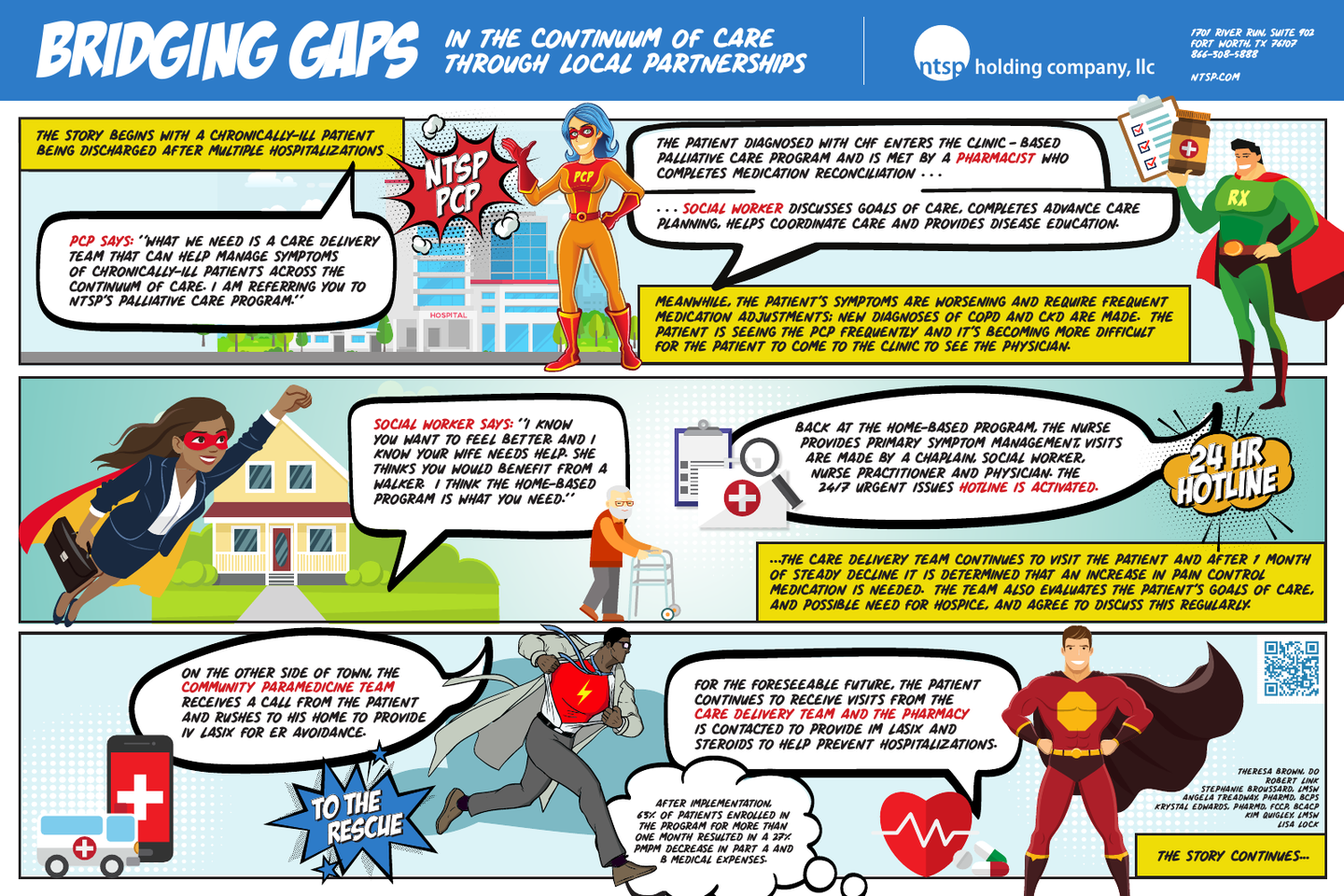
Bridging Gaps in the Continuum of Care through Local Partnerships
Objective:
Describe our program’s method and plan of identifying and bridging gaps in care for patients, and partnering with other agencies to provide service across the continuum of care.
Background:
NTSP Holding Company, LLC is an Independent Physician Association at global risk for over 80,000 Medicare Advantage members. The care delivery models include a care management company and a complete network of specialty and primary care providers (PCP). The palliative care (PC) program is administered through one of the company owned PCP clinics. The PC program was founded with the primary goal of improving care of chronically ill patients by managing symptoms. Other goals included reducing unnecessary and inappropriate medical care. Patients are usually referred to the program by their PCP, or by internal Care Management staff using our palliative screening tool. The clinic-based care is provided by a team which includes a physician, 2 social workers, and 2 clinical pharmacists.
Methods:
Common gaps in the continuum of care, such as medication issues, crisis management, caregiver stress, social isolation, care coordination and economic barriers, were identified by members of our team. These breaches in care resulted in our program being unable to efficiently care for patients in a shared-risk environment. Therefore, the need was recognized for partnerships to care for patients. After patients were identified, potential community partners were approached to maximize resources accessible to patients in order to close gaps.
Results:
Once contracting was completed, protocols and workflows were developed and implemented.
To support higher-acuity patients, the home-based program was outsourced to a partner organization which used its hospice-parent company’s infrastructure to build out a PC team (physician, nurses, social worker, and chaplain) and support the home-based patients with 24/7 triage and nurse care. Patients are selected for enrollment in the clinic or home program depending on their functional status and symptom management needs.
To reduce unnecessary or avoidable Emergency Department (ED) visits, both programs are supported by a community paramedicine program administered by the local emergency medical services (EMS) provider. To prevent unnecessary ED admissions, the home-program is further supported by a local 24-hour pharmacy for provision of medications in the home as needed during a crisis.
After implementation with partners, a per member per month (PMPM) cost reduction for 62.77% of patients enrolled greater than 1 month resulted in an overall PMPM reduction in Part A and Part B expenses of 26.93%.
Conclusion:
Local community partners have been instrumental in bridging gaps in the continuum of care for our PC patients. Our program has tried to take a member-centric view and provide care for the patient and their family across the continuum of care up until the doors of the hospital: from PCP and Care Management, and from lower acuity Clinic patients to higher acuity Home patients with EMS and pharmacy backup. Our next steps would be to focus on partnerships with local hospitals and skilled nursing facilities to better coordinate care during admissions and plan for discharges for these patients.
Author
Robert Link
Project Manager
NTSP Holding Company, LLC (North Texas Specialty Physicians)
1701 River Run, Suite 902
Fort Worth, TX, 76104
(817) 529-8296