CAPC’s Health Equity Accelerator
The Health Equity Accelerator, created and led by the Center to Advance Palliative Care (CAPC), is a year-long virtual program on how to design, implement, and sustain health equity initiatives for patients with serious illness.
The program launched in September 2025 at the CAPC National Seminar in Philadelphia, and includes 50 health care professionals from 19 states representing various backgrounds, perspectives, and lived experiences.
At the in-person workshop, participants learned:
- Best practices for planning, implementing, and monitoring the impact of a health equity quality improvement project—including how to garner needed resources.
- How to develop a personalized action plan aimed at advancing local health equity initiatives, including specific goals, strategies, and measurable outcomes.

Participants of the Accelerator will:
- Test an evidenced-based change management model. Participants receive training that follows a change management framework designed for health professionals to embark on projects to successfully address health inequities.
- Receive small group coaching. Each participant is assigned a health equity coach who will provide small group coaching throughout the program.
- Refine an action plan. Participants will continue to refine their action plan that advances an important strategic initiative that benefits their organization and partnering communities.
- Participate in topic-specific workshops. Virtual sessions will explore priority topics for advancing health equity and allow participants to interact with subject matter experts, gain exposure to emerging evidence and best practices, and explore specific approaches to improve care for individuals and communities.
- Connect with peers in idea exchange meetings. These CAPC-hosted quarterly sessions will provide an opportunity for participants to connect and support each other in advancing their initiatives and highlight the evolving work being led by the cohort.
- Monitor and evaluate project impact. Participants will complete a survey upon completion of the year-long program to capture information about progress of health equity initiatives, satisfaction with/usefulness of the Accelerator, and lessons learned to share with other health equity leaders.
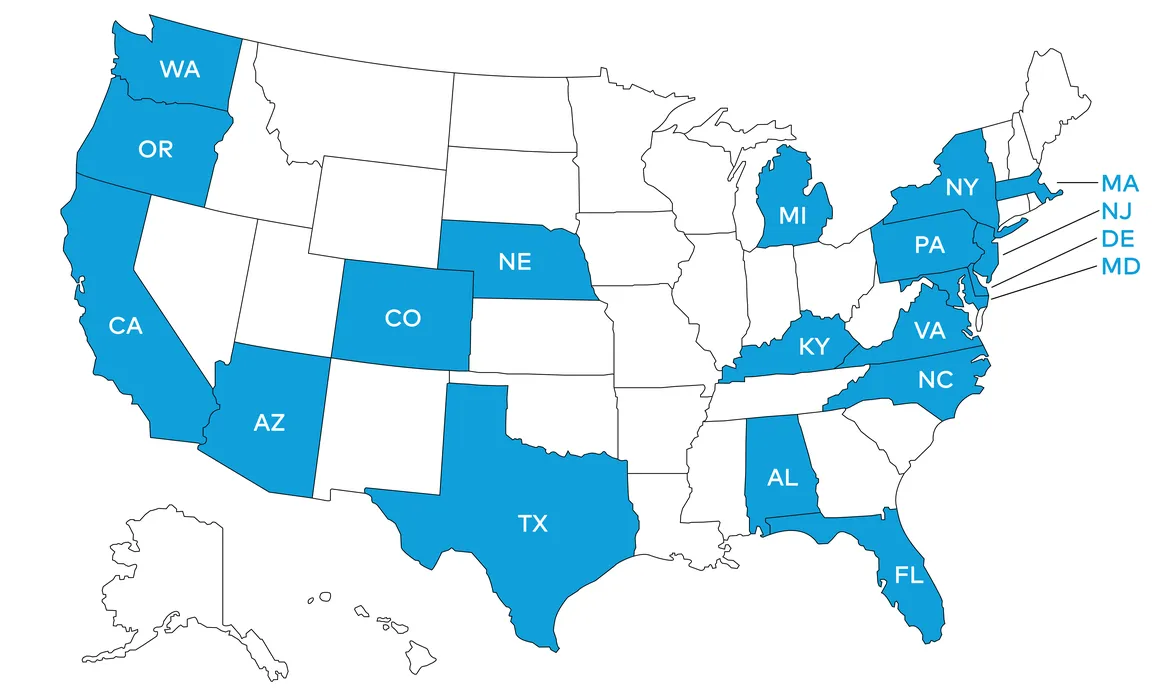
Where are Accelerator participants serving patients?
Accelerator participants are serving patients in 19 states across the country.
What challenges are participants planning to address with their health equity projects?
Access to Palliative Care
- Delayed or avoided referrals to palliative care due to misconceptions or lack of information; low utilization of palliative care in communities due to mistrust or lack of awareness; integration of palliative care into trusted community settings (e.g., free clinics, dialysis units)
- Geographic disparities, especially in rural, tribal, and underserved urban areas; transportation challenges and lack of infrastructure for patients with disabilities; language access and need for care in patients’ preferred language and education level
Marginalized Populations
Disparities for specific patient populations, including racially/ethnically diverse communities; LGBTQ+ patients; people with disabilities; unhoused individuals, justice-involved individuals, etc.
Communication and Health Literacy
Clinician communication skills, especially around goals of care conversations; lack of plain language in care and research materials; inclusive, non-discriminatory language in scientific and clinical communications
Research Inclusion
Underrepresentation in research of women, racial/ethnically diverse patients, and non-english speakers; lack of inclusive research practices, such as equitable compensation and feedback loops; bias in study design, data collection, and interpretation
Advocacy and Community Engagement
Task force involvement to advance equity initiatives; building alliances across backgrounds to expand reach and trust; focus on community-level impact
Why are Accelerator participants focused on advancing health equity?
- “In the 20 years since graduating medical school, I have maintained an awareness of the difference in health care received by the friends, family and neighbors that I grew up with vs. the highest levels of health care I was able to observe in my medical training. The more I have been able to learn about public policy and industry and its influence on health equity, the more I am able to see that the failing systems we have are performing as designed. We need to design the systems to work well for everyone, not just the lucky.”
- “Growing up in a rural community with limited access to health care, I witnessed firsthand the challenges of health inequity.… I became interested in health care early on, and by high school, I began to understand how factors like race, income, geography, and social connections could profoundly influence the quality and availability of care. This awareness has fueled my passion for advancing health equity and continues to guide my work in developing health care programs that prioritize inclusion, access, and justice.”
- “I first became passionate about advancing health equity during the COVID-19 pandemic, prior to moving to a career in hospice/palliative care. I was working in a nursing home and saw firsthand how the people I cared for and their families were disproportionately impacted by systemic barriers, especially limited access to resources and care…. In the past five years, I have become committed to advocating for more equitable approaches to care, especially for the individuals in our community who are underserved.”
- “...I am deeply committed to driving system change through data-informed strategies. I champion collaborative partnerships across interdisciplinary teams to build robust, accessible systems that ensure data integrity and transparency. ..I strive to make equity not just a goal, but a measurable and actionable reality within [my organization].
Accelerator Faculty
Komal Chandra, PhD
Vice President, Quality and Corporate Compliance
Niagara Falls Memorial Medical Center
Carine Davila, MD, MPH
Palliative Care Physician, and Director of Enrichment and Engagement, Division of Palliative Care and Geriatric Medicine
Massachusetts General Hospital
Marisette Hasan, BSN, RN
Vice President, Community Action & Policy
Coalition to Transform Advanced Care (C-TAC)
Arika Moore Patneaude, MSW, LICSW, APHSW-C
Director, Bioethics, Palliative Care and Journey Grief Support Programs
Seattle Children's Hospital
Andrya Rivera-Burciaga, DNP, FNP
Assistant Professor, Nurse Practitioner
University of Texas Rio Grande Valley - Nursing
Jackelyn Boyden, PhD, MPH, RN
Assistant Professor of Nursing - University of Pennsylvania
Children's Hospital of Philadelphia
CAPC Staff
Brittany Chambers, MPH, MCHES
Director, Health Equity and Special Initiatives
Rayna Ross, CHES
Health Equity Program Manager

This health equity initiative was made possible thanks to the generous support of the Arthur Vining Davis Foundations and the Rx Foundation.