The Results Are In: Palliative Care Professionals Share How They’re Doing in 2025

In early 2025, CAPC launched its second annual Palliative Pulse survey. The Pulse is our chance to ask palliative care professionals how they’re doing, their top concerns, and how we can help. Between late January and early March, more than 800 participants completed the survey, providing valuable insight into current professional needs. While this is not meant to be a representative sample, the results help guide CAPC decisions about the courses, technical assistance, and programs that we develop. In this blog, we share four key findings from participants’ self-reports and take a closer look at the data behind each one.
“It's the little moments that make the biggest impact. Like the patient who was bedbound but wanted to dance with her staff every morning, or having a family express gratitude for the care provided.”
This year, 854 palliative care professionals participated in the Palliative Pulse survey. About one-third (38.4%) worked for palliative care teams operated by hospitals, another third (36.8%) for teams operated by health systems, and the remainder for a mix of hospices, home health agencies, physician groups, and other organizations. Participants reported that their teams provided palliative care in all settings, with 75.5% providing care in the hospital.
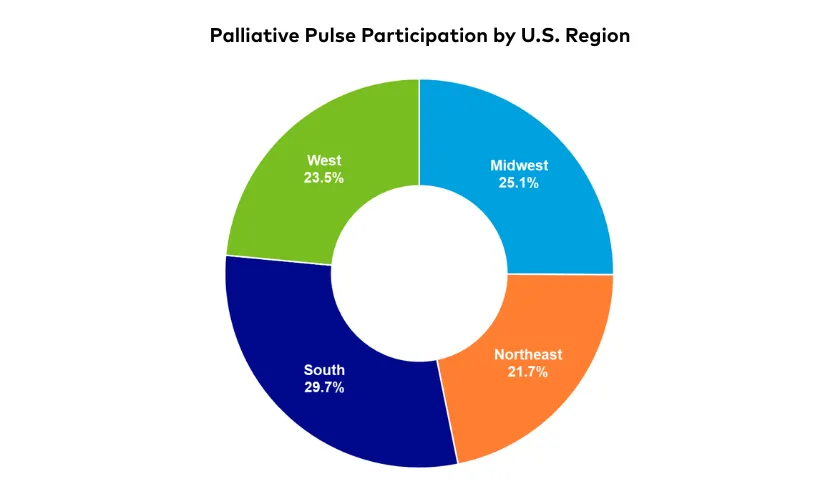
All U.S. regions were represented, with the largest share from the South (29.7%). Additionally, all patient age groups were represented, including 27.4% reporting that their patient populations included children with serious illnesses.
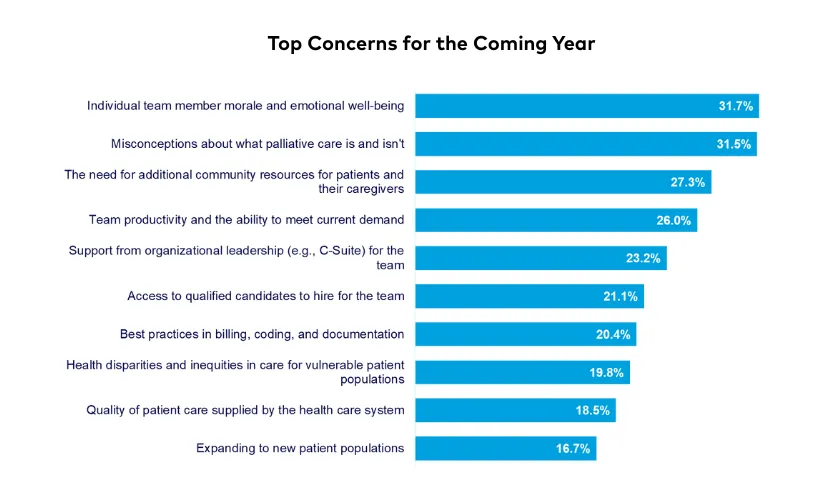
1. Team morale and emotional well-being are a top concern for the second year in a row
When asked to select their top three concerns for the next 12 months, nearly one-third of respondents (31.7%) selected “individual team member morale/emotional well-being," which was also the top selection in 2024. Two new answer options added this year, “misconceptions about palliative care” (31.5%), and “the need for additional community resources” (27.3%) rounded out the top three. These options replaced “team productivity” (26.0%), and “support from organizational leadership” (23.2%), which moved down into fourth and fifth place, respectively.
“The team is trained and skilled at listening to patients/families and not showing bias or judgment, but they are not always very good at using these skills within the team.”
Among those who self-identified as team leaders (n=309), the top three most-reported concerns were slightly different, with “best practices in billing and documentation” also a top concern (28.8%). While the sample size was small (n=10), participants who only treat pediatric patients’ top concerns included “access to qualified hires” (31.6%) and “health disparities” (28.9%).
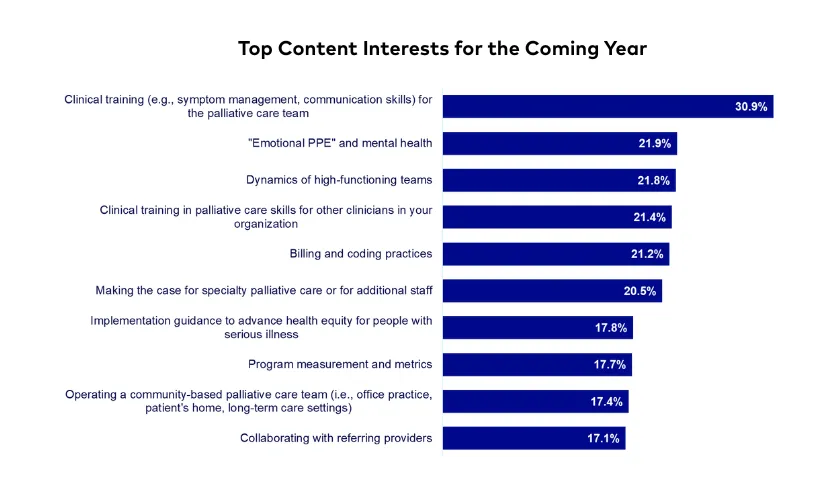
2. Clinical skills training is a top priority—for the palliative care team and for colleagues outside of palliative care
In both 2024 and 2025, clinical skills training was the top choice for what respondents considered to be valuable CAPC content. In the 2025 Pulse, the topic was split into two: “clinical skills training for the palliative care team” was the top choice (30.9%) and “clinical training in palliative skills for other clinicians” was in fourth place (21.4%). Other highly selected topics for educational content included, “emotional and mental health” (21.9%) and the “dynamics of high-functioning teams” (21.8%).
For team leaders (n=309), their top choices were “billing and coding practices” (31.1%), “program measurement and metrics” (25.9%), and “alternative payment models” (24.6%). And for respondents from pediatric-specific programs (n=10), there was a four-way tie for top concerns between “dynamics of high-functioning teams,” “emotional and mental health,” “program measurement,” and “making the case for palliative care/additional staff” (all 23.7%).
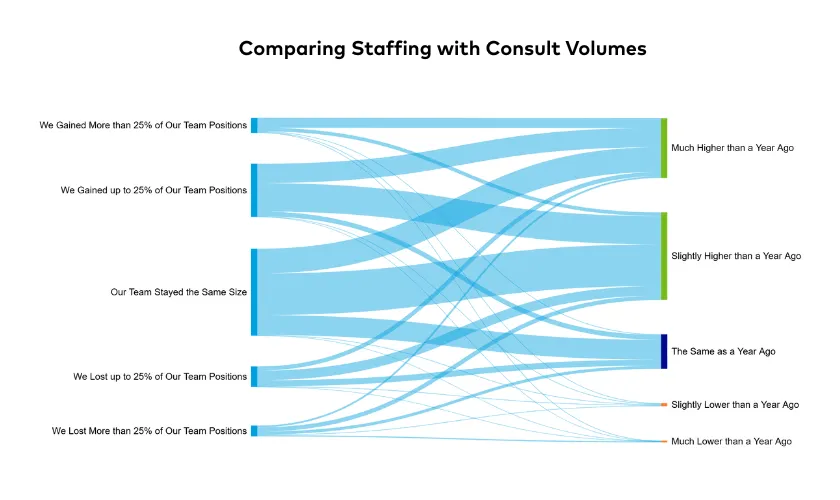
3. Consult volumes are climbing despite stagnant staffing levels
Nearly three-quarters of participants reported an increase in their team’s consult volumes since the prior year, while 22% said consult volumes stayed the same. Almost half of team leaders (46.6%), however, reported that their teams had stayed the same size—while 36.6% said that their team had gained staff positions, and the remaining 16.8% reported staff reductions. When we look at just the respondents who said that their team size had not changed (n=144), 76.4% still reported an increase in consult volume (and these increases were even reported by some team leaders who had lost staff positions).
4. Concerns for program sustainability have lessened since 2024, while perceptions of how much palliative care is valued have remained stable
The overall proportion of team leaders (n=309) who reported some level of concern for program sustainability decreased from 92.5% in 2024 to 86.1% in 2025. (Note: the survey was completed before any federal budget actions had reached the news.) About one-third (33.7%) were extremely (or quite) concerned, down from 42.5% last year.
"When a patient, family member, or colleague says, 'What would we do without you?’"
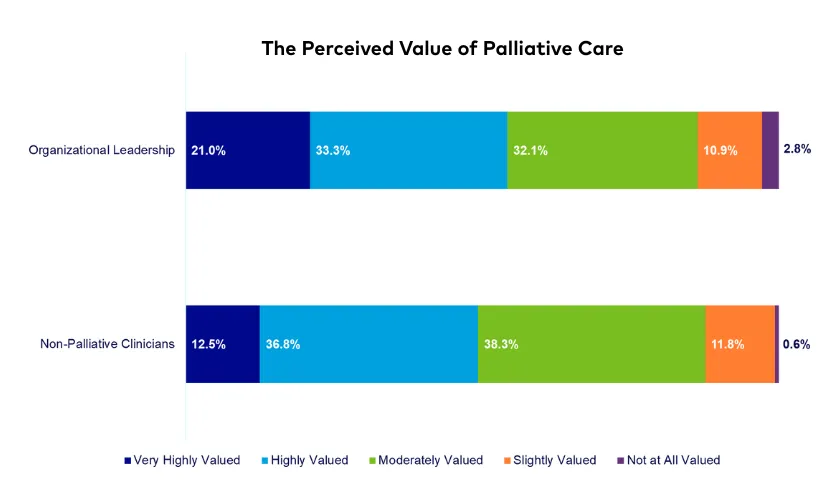
There was very little change, however, between 2024 and 2025 in the perceived value of palliative care by organizational leadership and non-palliative care providers. In 2025, 54.2% participants felt that their organizational leaders highly (or very highly) valued the palliative care program, as well as 49.3% reporting high value among non-palliative care providers. Among leaders who felt their palliative care programs were valued (or highly valued) by organizational leadership (n=169), more than a quarter (27.8%) were still very concerned for their program's sustainability.
Conclusion
The Palliative Pulse survey is an invaluable opportunity for CAPC to hear from our constituents. We are grateful to you for taking the time to complete the survey—we want you to know we are considering your responses in everything we do. Based on what you’ve told us, CAPC is developing new tools and programs focused on professional well-being, billing and coding, making the case for program resources, and other key topics raised in your responses.
We look forward to sharing these resources with you and hope you’ll consider adding your voice again in our 2026 Palliative Pulse survey.

Be the first to read articles from the field (and beyond), access new resources, and register for upcoming events.
SubscribeEdited by Melissa Baron. Clinical review by Andrew Esch, MD, MBA.
