The National Palliative Care Registry™: Trends in Hospital Palliative Care Since 2008
The National Palliative Care Registry ™, established in 2008, is a joint project of the Center to Advance Palliative Care (CAPC) and the National Palliative Care Research Center (NPCRC). With the expansion of palliative care programs over the past two decades, CAPC and NPCRC recognized the need to track the growth of the discipline nationally and establish a mechanism to collect information on palliative care teams, operations and service delivery.
Since the Registry’s start, approximately 400 hospital programs have participated each year, giving them access to reports that track their own program’s growth over time and compare their program’s characteristics to those of peer programs across the nation.
Palliative care programs have used Registry reports to secure needed resources for the delivery of high quality palliative care in their hospitals. CAPC, NPCRC and other organizations use the Registry data to make the case for increasing access to palliative care nationally, ensuring adequate staffing levels, promoting professional certification in palliative care and establishing reference points for operational and outcomes metrics.
Now, with eight years of data, we can see the growth in hospital palliative care and examine some of the key trends in staffing and operations. Here is an overview of some of these trends – and some areas where the field still needs to improve to ensure that all patients who need it are receiving high quality palliative care for themselves and their families.
Expanding Access to Hospital Palliative Care
Palliative care service penetration (the percentage of annual hospital admissions seen by the palliative care team) is a measure that illustrates how well programs are reaching patients in need. Palliative care programs submitting data to the Registry have achieved a steady increase in average palliative care service penetration, nearly doubling from 2.6% in 2008 to 4.8% in 2015.
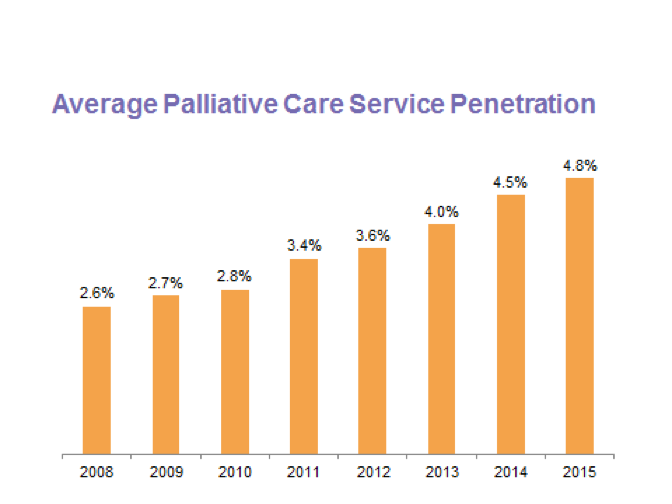
Researchers and providers estimate that approximately 10% of hospitalized patients may benefit from a palliative care consultation, varying depending on the hospital’s patient population. The 2015 average is approaching this minimum threshold, and one in ten programs report penetration rates of 8.7% and higher. This steady increase in penetration demonstrates improvements in access to palliative care in hospitals and helps programs to track their own ability to reach patients in need, set benchmarks and identify areas for improvement.
Similarly, the Registry measures changes in staffing – both in terms of team size and composition. In 2015, hospital palliative care teams had an average of 5.4 full-time equivalent (FTE) staff, an increase from the 3.2 FTE reported in 2008. The percentage of programs reporting a complete core interdisciplinary palliative care team (physician, nurse, social worker and chaplain) has also increased from 30% in 2008 to 44% in 2015. While nearly half of all palliative care programs participating in the Registry now have a complete interdisciplinary team, there is room to grow.
Improving the Quality of Palliative Care
Timing of palliative care is associated with quality—consults occurring in the first few days of a hospitalization are associated with measurably better outcomes. To assess timeliness, the Registry tracks the average time from hospital admission to palliative care consultation. To assess the types of patients served, the Registry reports on palliative care program integration with the intensive care unit (ICU) as well as patients’ primary diagnosis.
Palliative care teams have shown progress in reducing pre-consult length of stay (the average number of days from hospital admission to palliative care consultation). For patients discharged from the hospital, the average pre-consult length of stay dropped from 5.6 days in 2012 to 4.9 days in 2015. Nonetheless, most programs are still far from the recommended pre-consult length of stay of 2-3 days. In 2015, only one in five programs reported a mean time to consult of 3 days or less.
Reliable integration of palliative care in critical care settings is another measure of quality for palliative care and half of Registry programs are reporting collaboration with hospital ICUs. Forty-eight percent of programs report collaboration, and 17% report that the ICU has its own palliative care plans in place. Seeing a mix of patients by diagnosis is also an indicator of quality in terms of integration of palliative care across the hospital. In 2009, 35% of all patients referred to palliative care had a primary diagnosis of cancer; in 2015, this was down to 29%, reflecting expansion to other serious illnesses. Additionally, more patients seen by the palliative care team are able to leave the hospital, an increase from 71% in 2009 to 78% in 2015, suggesting that palliative care is expanding upstream during the course of illness.
Expanding the Registry
In the next two years, the National Palliative Care Registry™ will build the same strong evidence base for palliative care across the continuum of care, with surveys and reports not only for hospitals, but now including palliative care services in the home, office practices and long-term care settings.
For more information on U.S. palliative care, go to registry.capc.org and review our most recent presentation, outlining the latest trends in hospital palliative care. Stay tuned for the 2015 National Palliative Care Registry™ Trend Report, to be published in October.

