How to Drive Program Growth with Data from the National Palliative Care Registry
It has been my experience that palliative care teams work from their hearts, and though the work can be emotionally exhausting, they keep going, and keep giving of themselves. This can sometimes result in feeling overworked and burnt out. Without the right data, it can be hard to gauge whether these feelings are due to the natural demands of palliative care or if, in fact, workload is too high and additional staff are needed.
The data can provide the “back-up” to anecdotal stories supporting the team’s observations and experiences of feeling understaffed and bordering on burn out. The data can also demonstrate the value of your palliative care program. This article explains how I used national data to show that my team was providing high-quality palliative care, and also seeing substantially more patients than the average team—and those data led to growth in our program’s staff.
The process for requesting additional staff can be a stressful one, particularly in a climate where there is hesitation to approve positions that are non-revenue generating (i.e., palliative care doesn’t “make money”). Knowing the odds were against me, my very short “elevator speech” to the Staffing Committee had to be chock full of irrefutable data and honed to perfection. At the end of that five-minute presentation, I had approval for a full-time Nurse Practitioner and a Pool Nurse (1.2 FTE’s). Here’s how I did it (and you can, too).
Define the gap, and propose a solution:
Example: “The palliative care team is operating well below national average staffing levels. Palliative care consults per FTE were 335, while the national average is 251. Hiring an additional clinician would allow us to…”
Determine which metrics matter to key stakeholders:
Perform a mini needs assessment with key stakeholders in your organization. Then, demonstrate how expanding your service will address the needs of the greater organization.
Example: If stakeholders say, “We are focused on reducing 30-day readmissions for COPD patients,” then be sure to include some national data that speaks to the benefits of palliative care in COPD in your proposal. Consider a retrospective review of your data to quantify the percentage of patients with COPD that received a palliative care consult, then analyze their disposition and/or readmission rates.
Arm yourself with some evidence-based talking points to showcase the value of palliative care, and combine them with your local data to strengthen your case.
Conduct a literature review:
Don’t underestimate the benefits of a comprehensive lit review: it helps ensure that you are a subject matter expert. Arm yourself with some evidence-based talking points to showcase the value of palliative care, and combine them with your local data to strengthen your case. You can get started here.
Collect and analyze data:
A common issue palliative care programs face is finding the time to collect and analyze data on their program’s characteristics and impact (numbers of patients served). However, taking the time to measure your performance provides data that are essential to justifying growth.
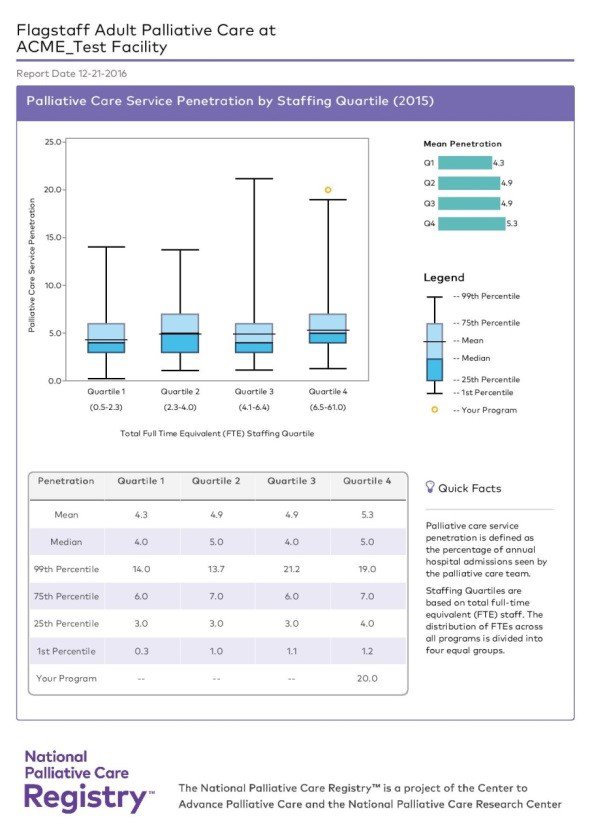
Supporting data for your program are easily accessible on the National Palliative Care Registry™. The Registry is free and will provide you with impressive charts and graphs, comparing your program to national averages/medians. Examples of information available:
- Service Penetration – what percentage of patients your palliative care program serves
- Interdisciplinary Team Workload – number of consults per FTE (this one made jaws drop in my hospital!)
- Length of Stay (LOS) by Hospital Size – illustrates time to palliative care consult and time to discharge
Enlist the help of your organizations’ data experts (you may have to treat them to coffee or chocolate). I was shocked at how much of the information requested for the Registry was already being collected. Enter as much of your program’s data as you can—you won’t regret the investment of your time when you see how your program stacks up nationally.
Demonstrate value:
The literature demonstrates the positive outcomes of palliative care involvement in helping to achieve the Triple Aim: better health and better care at a lower cost. Utilize data and graphs that illustrate your program’s quality. One of the ways I demonstrated value was by aligning data collection with best practices, such as the National Quality Forum (NQF).
Examples: % of palliative care consults screened for pain and dyspnea (NQF 1634 & 1639); % with documented goals of care (NQF 1641)
Don’t forget about the $$$! Opportunities for revenue and cost savings:
Clinicians (usually MDs, APRNs, and PAs) providing billable services (check with your Billing Specialist as it varies by state) present an opportunity for revenue generation. Estimate the potential number of new consults and follow-up visits and reimbursement to demonstrate ability to offset salaries.
Check to see if your organization has an estimate for cost savings per palliative care consult. If not, you can use national estimates for cost savings from your literature review, or utilize the CAPC Palliative Care Impact Calculator.
A study conducted by Trinity Health estimates a cost savings of $1,670 per inpatient palliative care consult—multiplied by the estimated number of new patients, the cost savings alone may cover the cost of the clinician, and then some!
Example: Request for an NP (these numbers are just an example of the math, please consult your Billing and Finance departments)
- Potential to see 400 new patients per year
- 400 new patients x $1,670 cost savings per patient = $668,000 annual cost savings
- PLUS $XX,000 estimated annual billing
Put it all together into a written summary, and go make your case!
If at first you don’t succeed, try, try again:
I submitted proposals to hire a Medical Director several years in a row before winning approval. (However, come to think of it, that was before I had the Registry data to support my requests.) Sometimes, it’s just not the right time. Changes in leadership, changes in priorities, and financial fluxes can all impact the outcome. Try again later.
Reminder:
You will be grateful that you entered your program’s data into the Registry. I often cite statistics that I learned from the Registry; and I include one or two Registry graphs in every white paper, FTE request, and strategic plan that I write. It has contributed greatly to our credibility as a medical subspecialty and service line. It has also directly led to our ability to provide palliative care to more patients. So take the time, gather the data, and go make the case.

The National Palliative Care Registry™ serves palliative care programs across the continuum of care and is free and open to all. Participating in the Registry gives you access to customized reports on how your program compares to other programs across the country, including penetration, staffing, length of stay, and more.
The Registry is a joint project of the Center to Advance Palliative Care and the National Palliative Care Research Center. Learn more.
