What's the Score? Using a Mortality Risk Score to Support Program Growth
Competing for limited C-suite resources is a challenge for all Palliative Medicine (PM) program leaders. While it is well understood that there are substantial unmet needs in the community that could be addressed with the addition of more resources, executive leaders often require objective ways to demonstrate this need – including the estimated increase in case volumes that would result by adding more providers. Our system relies on per-case cost savings analysis to help support PM resource allocation, so any request for program growth must have valid projections as to the expected case increase with the addition of more PM resources.
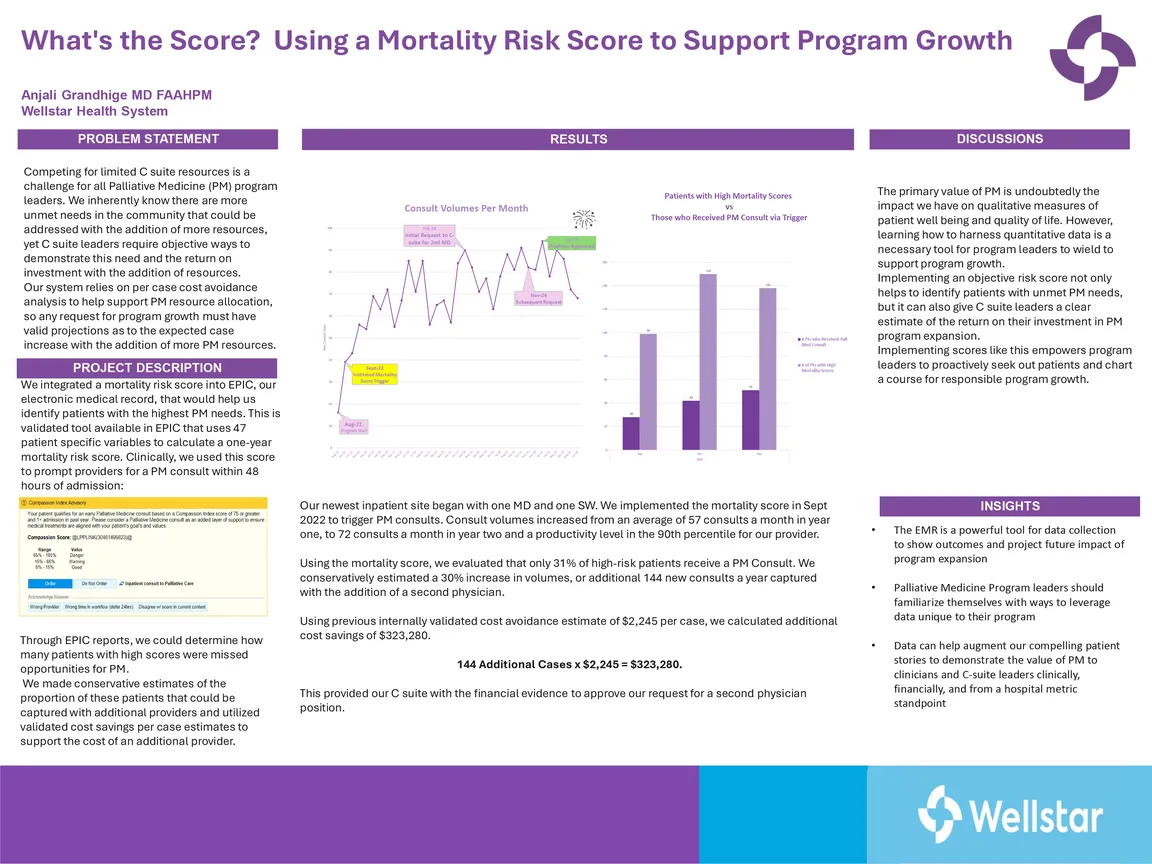
We integrated a mortality risk algorithm developed by EPIC, our electronic medical record, to help us identify patients with the highest PM needs. This score uses 47 different patient specific factors to calculate a one-year mortality risk score. Clinically, we used this score to prompt providers for a PM consult within 48 hours of admission. Through EPIC reports we could evaluate what percentage of high-risk patients received a PM consult, and how many were missed. We then made estimates of the proportion of patients that could be captured with additional providers and utilized validated cost savings per case estimates to support the cost of that additional provider.
Our newest inpatient site began with one physician and one social worker. We implemented the mortality score to trigger PM consults. This quickly increased consult volumes from an average of 57 consults a month in year one, to 72 consults a month in year two and a productivity level in the 90th percentile for our provider. Using the mortality score, we evaluated the number of high-risk patients missed and conservatively estimated an additional 144 new consults a year captured with the addition of a second physician. We calculated additional cost savings of $323,280 using previously validated cost avoidance estimate of $2,245 per case. This provided our C-suite leaders with the financial evidence to approve a second physician position.
The primary value of palliative medicine is undoubtedly the impact we have on qualitative measures of patient well-being and quality of life. However, learning how to harness quantitative data is a necessary tool for program leaders to wield to support program growth. Implementing an objective risk score not only helps to identify patients with unmet PM needs, but it can also give C-suite leaders a clear estimate of the return on their investment with PM program expansion. Implementing scores like this empowers program leaders to proactively seek out patients, demonstrate value, and chart a strategic pathway for dynamic program growth.
Author
Anjali Grandhige, MD, FAAHPM (Wellstar Health System)