The Science, Art, and Heart: Bringing Palliative Care Education to the Bedside
Acute Care nurses are often left feeling uncomfortable, inadequate, or unsure of how to best care for palliative and end of life patients. Pre-licensure education lacks sufficient training in palliative care tenants and principles, including end of life care. The National Consensus Project (NCP) (2018) states that palliative care should be available to all populations across the lifespan and across all health settings. The Institute of Medicine (IOM) (2014) highlights a critical need for a focus on improving end of life care indicating that by providing high quality healthcare services to patients and their families, an enhanced quality of life and “a more sustainable care system” could result. In addition, the IOM points out the need to address challenges such as an inadequate number of educated providers specializing in this care, inequitable access, and the unsustainable cost of healthcare delivery in the U.S. (Institute of Medicine [IOM], 2014, p. 4). Main Line Health System has committed to support bedside staff with evidence based, palliative care focused education.
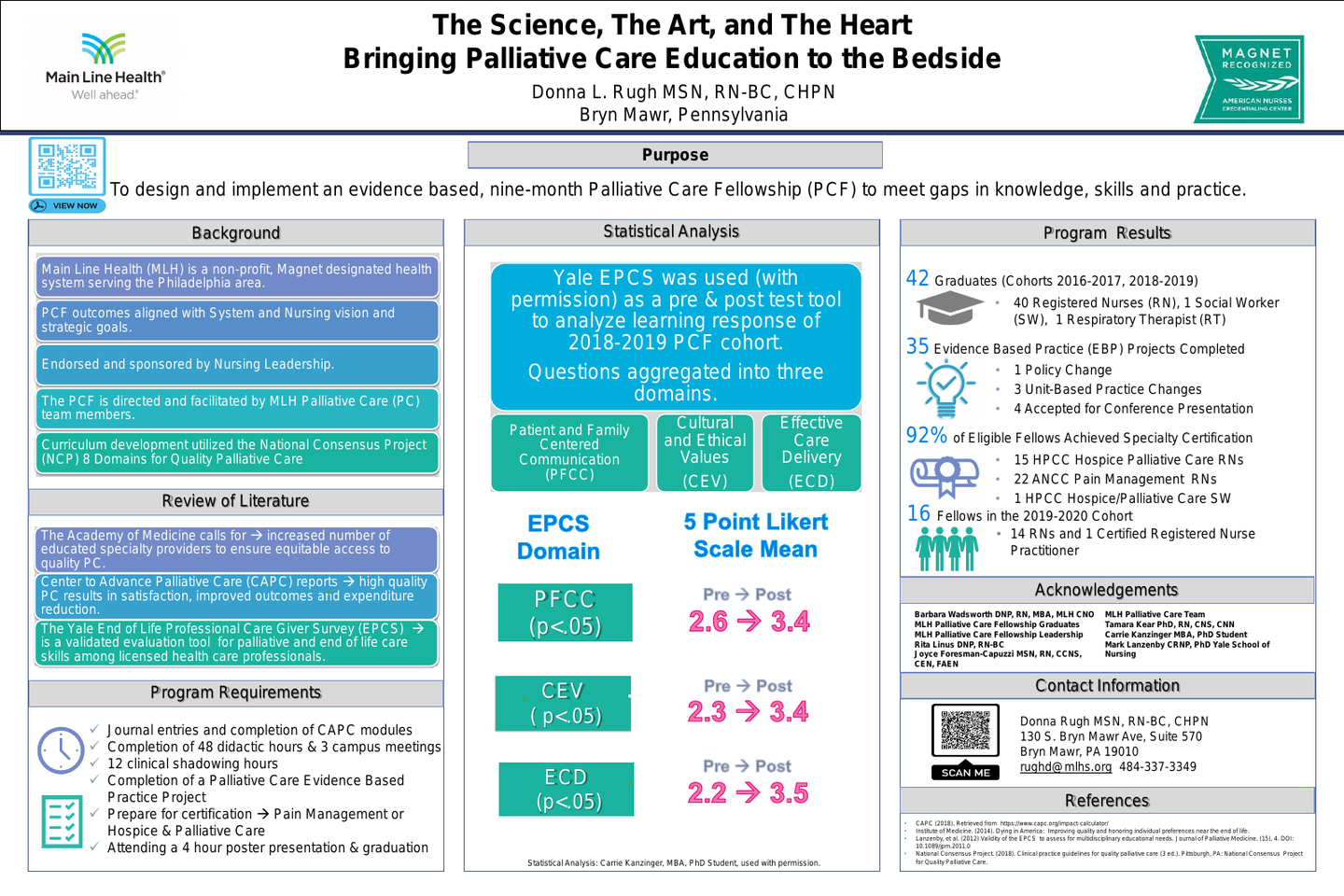
Our evidence-based Palliative Care Fellowship is directed and produced by palliative care team members. Two years of bedside experience, completion of the End of Life Nursing Education Consortium (ELNEC) curriculum, an application, and an interview process are required prior to consideration. The Main Line Health Palliative Care Fellowship emphasizes enhancing open communication, skilled delivery, and increased comfort in providing proactive and equitable access to palliative care at the bedside and beyond for patients and families affected by life-limiting illness.
Our palliative care fellows are expected to aspire to a higher level of professional practice through advanced critical thinking, motivation, and vision. Success is measured through pre and post surveys, anecdotal reports, achieving specialty nursing certification, and completing an evidence-based practice project.
Since 2017, the system-wide program has graduated more than 40 bedside staff members. Over 90% achieved specialty nursing certification in either Pain Management or Hospice/Palliative Care. Collectively, the fellows completed 25 evidence-based projects.
Permission was obtained and The Yale End of Life Professional Caregiver Survey (ECPS) was used to evaluate the effectiveness of the 2018-2019 program. Results showed significant statistical improvement in the mean score pre and post intervention for all domains:
Patient and Family Centered Communication (t41.862= -5.824, p < .05)
The mean difference in domain score was 9.050 higher post-intervention
Cultural and Ethical Values (CEV) (t33.729= -5.366, p < .05)
The mean difference in domain score was 6.360 higher post-intervention
Effective Care Delivery (ECD) (t38.700= -6.034, p < .05)
The mean difference in domain score was 7.470 higher post-intervention
Author
Donna Rugh, MSN, RN-BC, CHPN
Main Line Health Nurse Educator Palliative Care/Pain Management, Palliative Care Nurse Coordinator
Main Line Health System
Bryn Mawr Hospital/Palliative Care Department
130 S Bryn Mawr Ave, Suite 570
Bryn Mawr , PA 19010
(484) 337-3349