Rising Like the Phoenix: Leadership Methods for Restoring Team Morale and Purpose
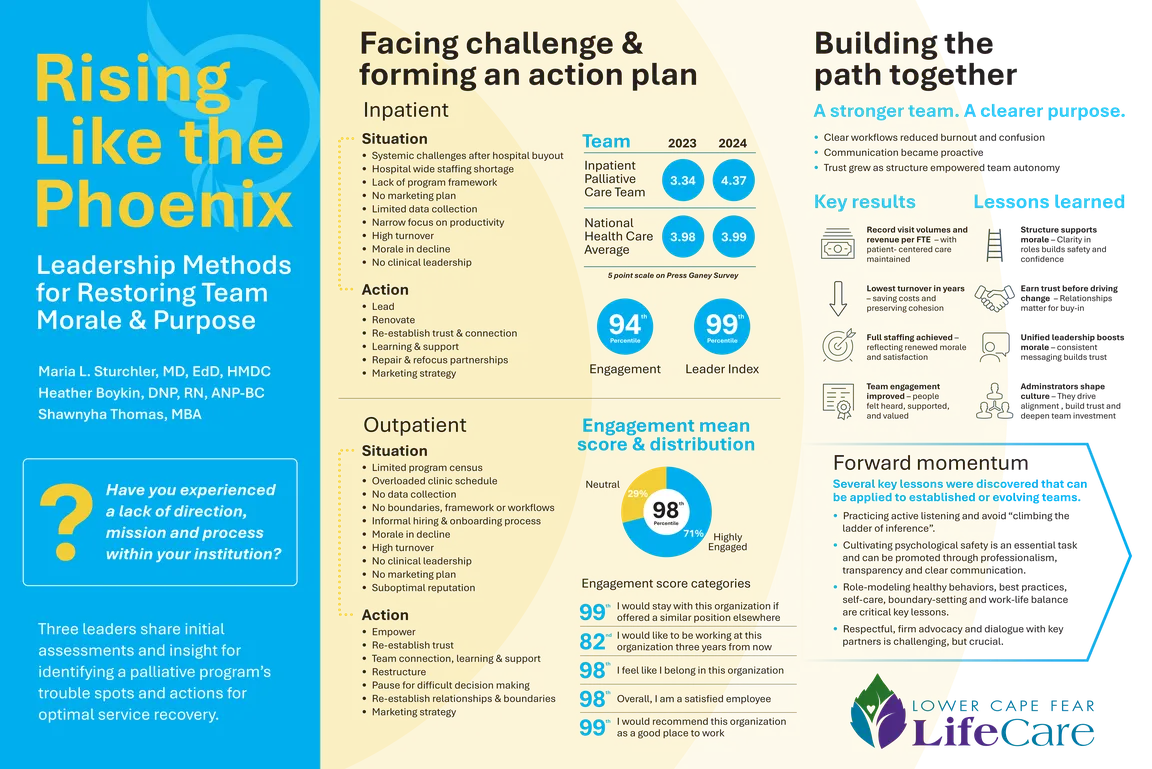
Palliative care teams experiencing low morale and burnout often exhibit emotional exhaustion, detachment, and a diminished sense of professional accomplishment. Continuous exposure to suffering, high patient mortality, and heavy workloads can cause compassion fatigue and frustration, leading to low morale. This can cause team members to feel unsupported, overburdened, or undervalued, ultimately negatively impacting collaboration and patient care quality. Over time, burnout can erode job satisfaction, leading to high turnover rates and emotional distress. The clinical and administrative leaders of our inpatient and outpatient palliative care teams aimed to address the demoralization and low staffing they encountered when starting in their roles in 2023. The teams' culture was in disarray, and record-high turnover was occurring in both departments.
Addressing these challenges required strong leadership, peer support, self-care initiatives, and organizational commitment to fostering a resilient and well-supported team environment for both inpatient and outpatient groups, despite the operational and logistical differences inherent in the work of each group. Through strategic planning with key partners, ongoing advocacy efforts, and prioritization of educational initiatives, process standardization has occurred on many fronts. Increased investment in team members has enhanced perceptions and optimized overall performance. We successfully advocated for certain resources to be assigned, or in some cases, reallocated and secured, to be leveraged on both teams for ongoing improvement efforts.
We observed and measured, in parallel groups, that team culture, morale, and engagement increased significantly through qualitative and quantitative indicators. Our annual employee engagement survey demonstrated unprecedented year-over-year improvements in both teams’ reported Leadership Scores and Engagement Scores. Furthermore, team turnover is at a historical low for both inpatient and outpatient palliative care teams. Absenteeism has dropped considerably, while peer recognition has strengthened, and collaboration and patient quality metrics are at all-time highs. Finally, more staff than ever before have expressed interest in pursuing advanced training, teaching opportunities, and other initiatives that demonstrate increased bandwidth and engagement due to improved team morale and work conditions.
Several key lessons have been noted by us through our experiences that can be applied to other teams. Practicing active listening and avoiding “climbing the ladder of inference” are crucial steps in obtaining necessary data from team members about which matters are most urgent. Cultivating psychological safety is an essential task, and can be promoted through professionalism, transparency, and clear communication. Role-modeling healthy behaviors and best practices in clinical and interpersonal matters, as well as self-care, boundary-setting, and work-life balance are additional key lessons. Finally, respectful and firm advocacy and dialogue with key partners is a sometimes challenging, but crucial, lesson learned in our experiences.
Authors
- Maria Sturchler, MD, EdD, HMDC (Lower Cape Fear LifeCare – Wilmington)
- Shawnyha Thomas, MBA, PPMC (Lower Cape Fear LifeCare – Wilmington)
- Heather Boykin, DNP, ANP-BC (Lower Cape Fear LifeCare – Wilmington)