Quality of Hospital Comfort Care without Specialty Palliative Care Involvement
The project reviews comfort care (CC) orders for patients who did not receive specialty palliative care (SPC) to identify and evaluate generalist palliative care in the hospital. Palliative care focuses on managing symptom burden in acute and chronic serious illness, addressing goals of care (GOC), and supporting both patient and families or other caregivers. Recent studies have shown improvement of patient outcomes with early palliative care involvement. The ability to conduct and appropriately document a thorough GOC discussion is imperative for the advocacy of patients and can be performed by non-specialty palliative care providers. This project aimed to evaluate services related to the transition to CC and how non-specialty palliative care providers currently document this transition.
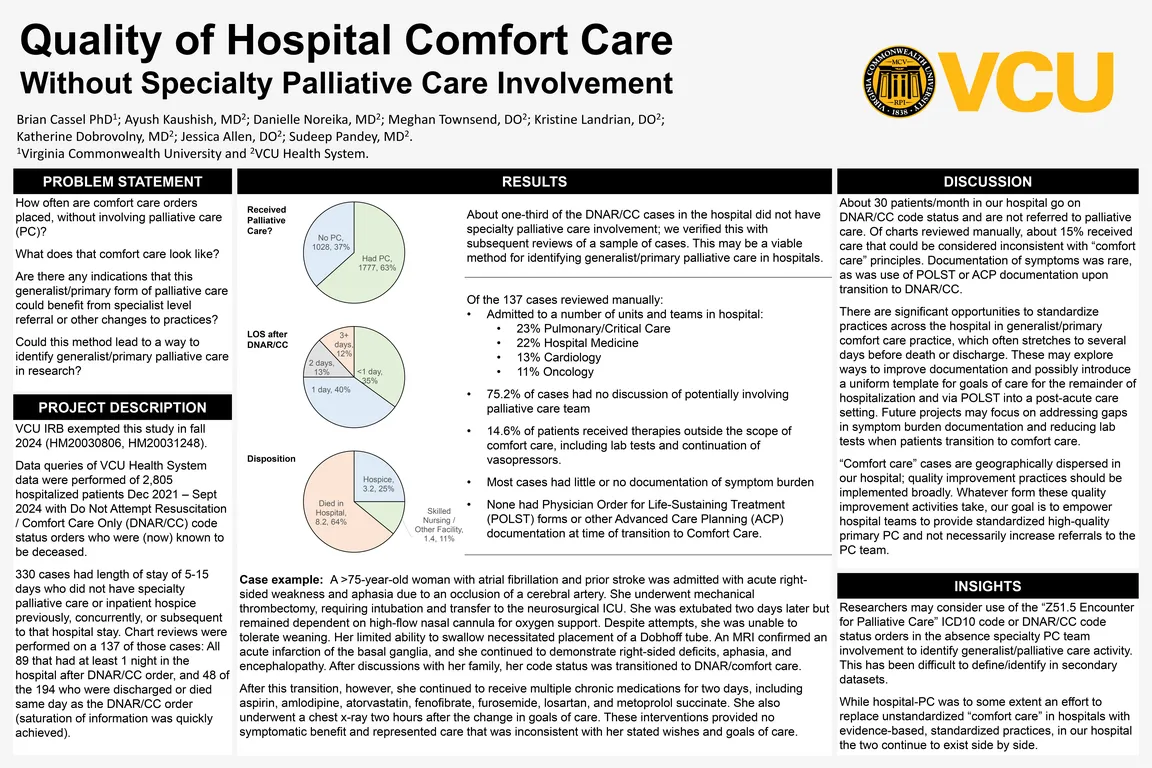
This is a retrospective quality improvement study with data collected from a large Level 1 trauma center between December 2021 and September 2024. Data queries were used to identify adult patients who had Do Not Attempt Resuscitation/Comfort Care (DNAR/CC) orders during a hospital stay, and whether they received SPC. 137 cases were selected for review which had an active DNAR/CC order set and did not have a specialty palliative care consult, had a length of stay of 5 to 15 days, and were now known to be deceased. We reviewed charts for appropriate code status history and changes, mention of palliative care services, symptom burden and treatments of symptoms, documentation of invasive or aggressive measures not aligned with comfort focused care, and total length of hospital stay.
2,805 adult hospitalizations had a DNAR/CC order. 1,777 (63.3%) had SPC involvement and 1,028 (36.7%) did not. Of the 137 cases reviewed, ages ranged from 27-99 years (mean of 67). Pulmonary, Cardiology and Hospital Medicine had the highest volumes. 70% died in the hospital, 22% were discharged to hospice, and 8% were discharged to a Skilled Nursing Facility or other facility. 75.2% of cases had no discussion of potentially involving SPC, and 14.6% of patients received therapies outside the scope of CC, including lab tests and continuation of vasopressors. DNAR/CC cases had little or no documentation of symptom burden, and none had Physician Order for Life-Sustaining Treatment (POLST) forms or other Advanced Care Planning (ACP) documentation at time of transition to CC.
We identified generalist palliative care successfully. Quality improvement projects are now underway to explore ways to improve documentation of goals of care, POLST, and ACP when SPC is not involved. Specifically, we are working to introduce a uniform template for goals of care for the remainder of the hospitalization which may continue via POLST to post-acute care. Future projects may focus on addressing the lack of symptom burden documentation and reducing the continuation of lab tests when patients transition to comfort care. These efforts may provide consistent documentation to reflect patient and healthcare power of attorney wishes and reduce the risk of unwanted invasive or aggressive measures. Our goal is to empower hospital teams to provide standardized high-quality primary palliative care.
Authors
- Brian Cassel PhD (Virginia Commonwealth University Health System)
- Ayush Kaushish, MD (Virginia Commonwealth University Health System)
- Danielle Noreika, MD (Virginia Commonwealth University Health System)
- Meghan Townsend, DO (Virginia Commonwealth University Health System)
- Kristine Landrian, DO (Virginia Commonwealth University Health System)
- Katherine Dobrovolny, MD (Virginia Commonwealth University Health System)
- Jessica Allen, DO (Virginia Commonwealth University Health System)
- Sudeep Pandey, MD (Virginia Commonwealth University Health System)