Exploring the Need for Palliative Care in a Pediatric Value-Based Care Model
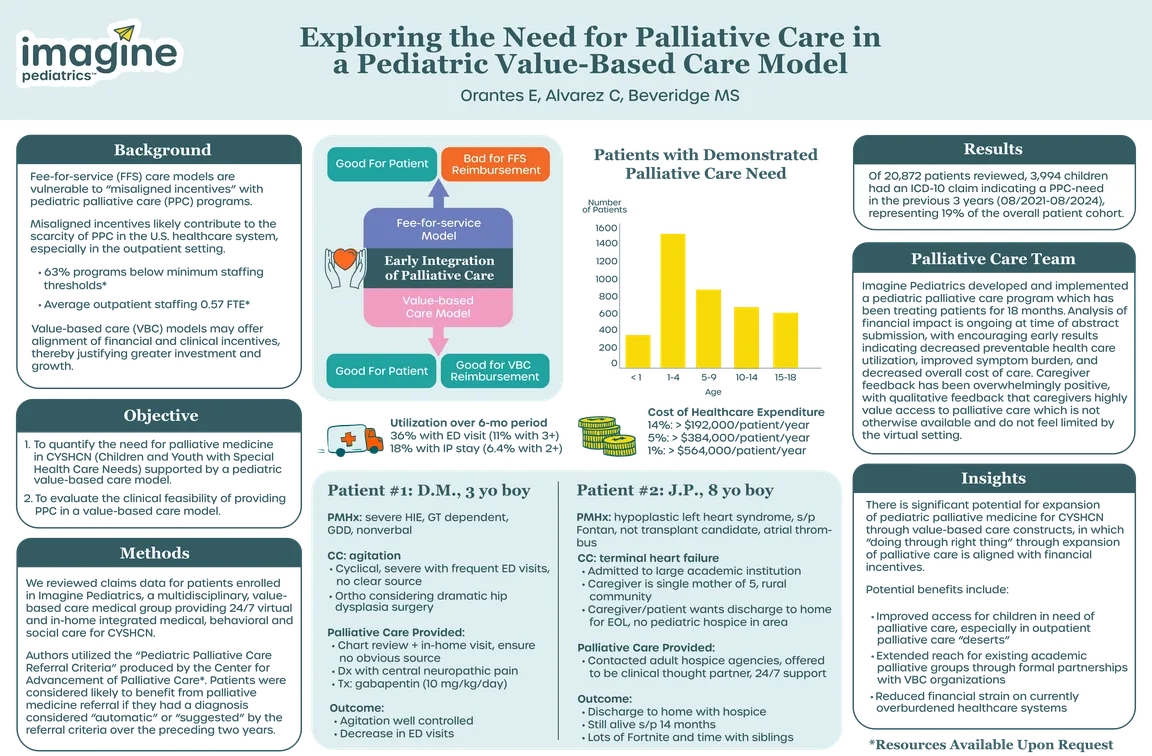
Pediatric palliative care (PPC) is well known to benefit children and youth with special health care needs (CYSHCN) through impacts such as improved quality of life, decreased symptom burden, and reduced caregiver distress. Despite this, there is an enormous scarcity of outpatient PPC programs. Traditional fee-for-service healthcare does not incentivize investment in PPC due to low reimbursement rates and time-intensive patient visits. In contrast, value-based-care (VBC) arrangements incentivize early implementation of community PPC due to the proven correlation with improved quality of care, decreased healthcare utilization, and reduced total cost of care. Despite this alignment, no studies have quantified the extent of clinical need in pediatric VBC arrangements.
We evaluated the need for PPC among CYSHCN supported by a pediatric VBC model. We reviewed claims data for patients attributed to Imagine Pediatrics, a VBC medical group providing 24/7 virtual and in-home integrated medical, behavioral and social care for CYSHCN via population-based contracts with managed care Medicaid payers. Children qualify for this service if they have sufficient medical complexity, as determined by an adapted version of the Pediatric Complex Chronic Condition Classification System. Authors utilized the “Pediatric Palliative Care Referral Criteria” produced by the Center to Advance Palliative Care (CAPC). Patients were considered likely to benefit from PPC referral if they had a diagnosis considered "automatic" or "suggested" by the referral criteria over the preceding 2 years.
Claims data were available for 20,872 attributed patients. Of those, 3,994 patients (19%) had a diagnosis that would benefit from PPC involvement. The palliative-eligible cohort was heterogenous in demography and pathology. As a result of this demonstrated need, Imagine Pediatrics implemented an outpatient PPC program that has seen patients for 18 months. Caregiver feedback has been very positive, with qualitative feedback that caregivers do not feel constrained by the virtual setting and value access to palliative care that would not otherwise be available to them. Analysis of financial impact is ongoing at the time of abstract submission, with encouraging early results indicating decreased preventable health care utilization, improved symptom burden, and decreased overall cost of care.
These results highlight the significant potential for expansion of PPC for CYSHCN through VBC constructs. Given the national shortage of PPC providers especially in the outpatient setting, there is a need for community-based palliative care services under value-base-care models, in which “doing the right thing” through expansion of palliative care is aligned with financial incentives. Expanding PPC services would not only improve quality of life for CYSHCN, but also alleviate financial strain on an already overburdened healthcare system. Ongoing work is needed to understand challenges for these emerging programs, including limitations of the virtual setting, communication and collaboration with academic programs, and evolving regulatory and legislative restrictions.
Authors
- Stockton Beveridge, MD (Imagine Pediatrics)
- Calista Alvarez, BSN, RN (Imagine Pediatrics)
- Elizabeth Orantes, PNP-AC (Imagine Pediatrics)