Evaluating the Use of Artificial Intelligence in Outpatient Palliative Care
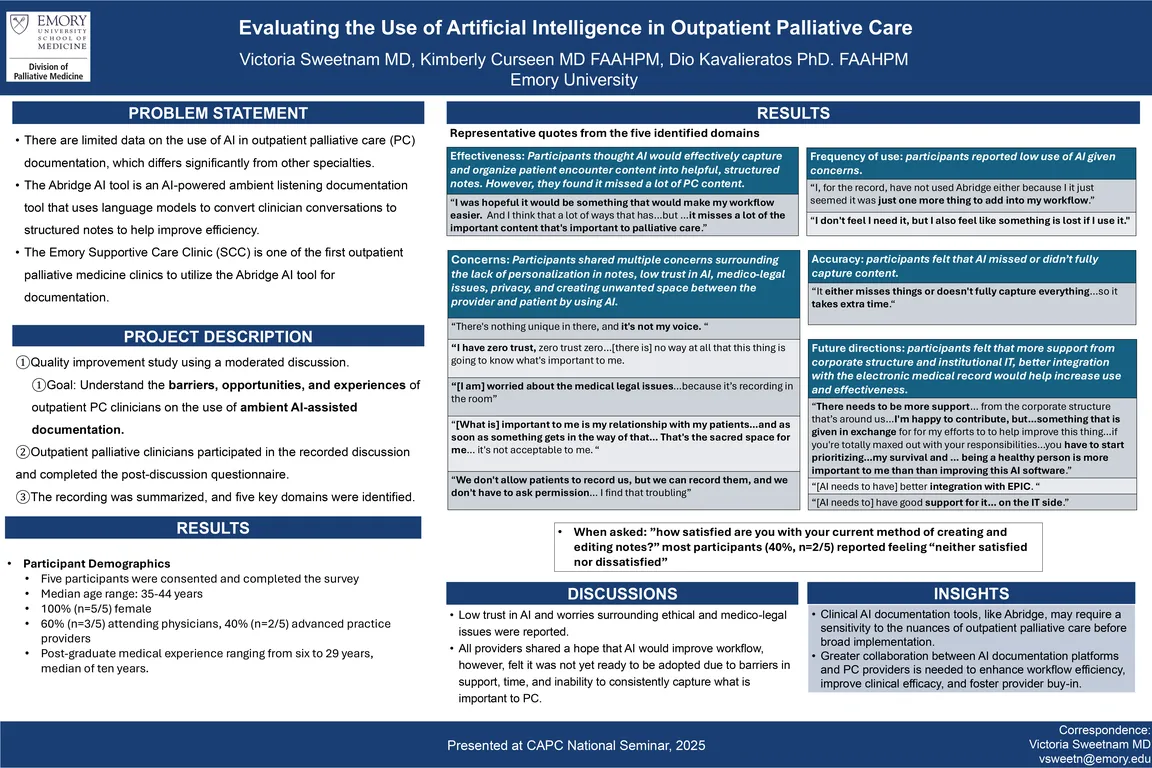
There are limited data exploring the use of Artificial Intelligence (AI) in palliative care documentation, as content in this specialty significantly differs from other specialties. One clinical resource developing popularity, called the Abridge AI tool (Abridge), has been created to improve efficiency in clinical documentation. However, it has not yet been studied in the palliative care literature. We aimed to gain providers' perspectives on the incorporation of AI in clinical documentation, as one of the first outpatient palliative clinics nationally to incorporate this tool.
In this quality improvement project, we convened a moderated discussion group of five outpatient palliative care providers at a single academic medical center. The interview guide addressed key domains of interest including provider perceived frequency, effectiveness, concerns, accuracy, and future directions of Abridge. Participants were invited to voluntarily participate in the recorded discussion and complete a survey. The recording was summarized, and key discussion themes were identified. The survey contained discrete items which were analyzed using descriptive statistics including medians and proportions.
Of the five outpatient palliative providers who participated, 60% were attending physicians and 40% were advanced practice providers. Post-medical graduation experience ranged from six to 29 years, with a median of 10 years. Some providers reported low trust in AI in general and shared their worries surrounding the ethical issues of its use. All providers expressed initial hope that AI would improve workflow, however they later reported that they found it frustrating that the AI tool “misses and ignores” content critical to palliative care, including advance care planning and psychosocial aspects of care. Additionally, providers felt that the AI-generated documentation did not “sound” like their voice, “that something is lost if I use it,” and that it required extensive editing.
In summary, providers shared that the AI documentation tool requires sensitivity to the nuance of palliative care practice before implementation to optimize efficiency and effectiveness in workflow. Participants reported that the tool was not yet ready for palliative care specific documentation and would need to be optimized before broad implementation.
Authors
- Victoria Sweetnam, MD (Emory University)
- Kimberly Curseen, MD (Emory University)
- Dio Kavaliertos, PhD (Emory University)