Enhancing Early Palliative Care for CHF and COPD: A System-Wide Initiative
This project addresses the late initiation of palliative care for patients with chronic conditions like Congestive Heart Failure (CHF) and Chronic Obstructive Pulmonary Disease (COPD), which often involve complex symptom management and progressive decline in quality of life. Despite the well-documented benefits of early palliative care, it is frequently introduced too late, leading to unnecessary hospitalizations, prolonged suffering, and care that is not aligned with patient preferences. The project advocates for early palliative care involvement, focusing on proactive goal setting, advance care planning, symptom management, and family or caregiver support. By integrating palliative care earlier in the disease trajectory, the project aims to improve patient outcomes, enhance quality of life, and reduce unnecessary readmissions and healthcare costs.
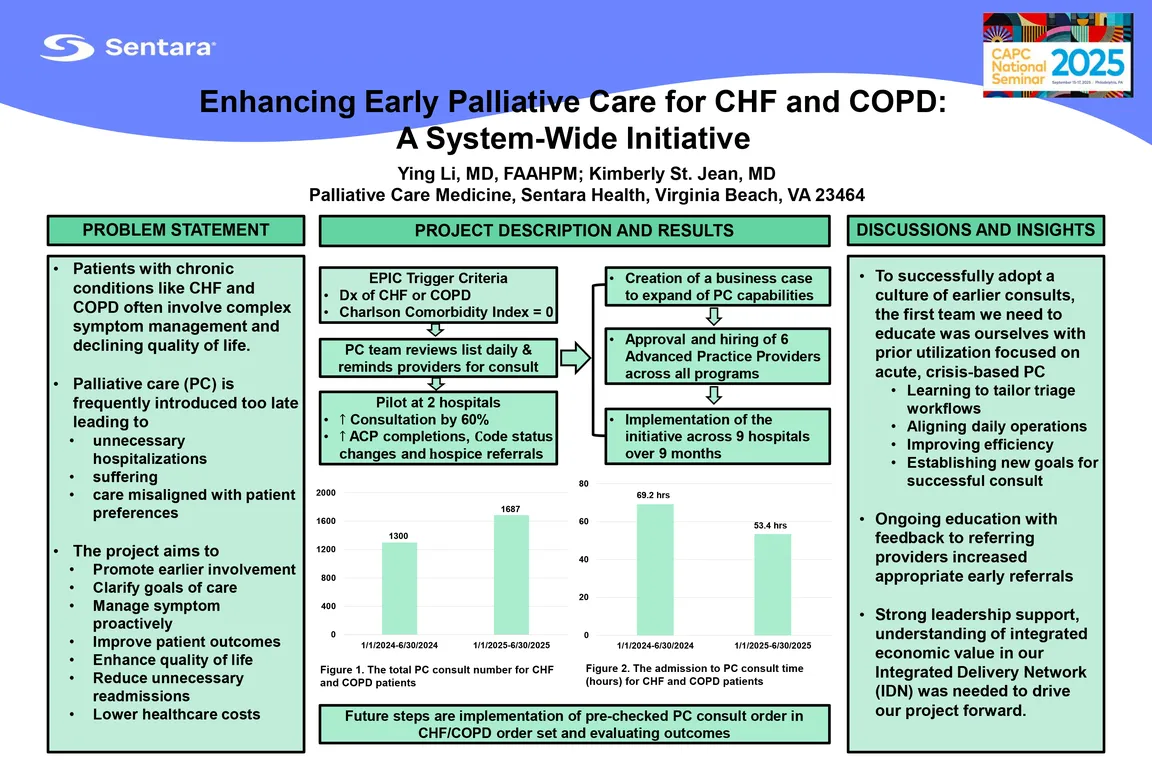
We piloted an initiative at two hospitals to increase the frequency of earlier, routine consultation to palliative care. Using the Charlson Comorbidity Index (score 0) in the electronic medical record (EMR), we identified high-risk patients with CHF and COPD for early referrals. Consults increased by 60%, resulting in significant outcomes such as advance care planning (ACP) completions, code status changes, do-not-resuscitate (DNR) completions and hospice referrals. The pilot also showed increased demand for palliative care services. Pilot data were combined with organizational metrics and palliative care literature to develop a business case showing the value of early palliative care to our IDN (Integrated Delivery Network). In addition to the business case, a plan was created for implementation at our 9 system hospitals, including additional advanced practice provider (APP) full-time equivalent (FTE) and process adaptation to support sustainable integration.
The project led to the approval and hiring of six APPs across all programs. Through strong collaboration with hospital leaders, hospitalists and specialists, the initiative was successfully expanded across nine hospitals over a nine-month period. This resulted in a 64% average monthly increase in consultations and a decrease in time to palliative care consultation. Due to this project, hospital medicine approved adding "palliative care consult" as a pre-checked option in the CHF and COPD admission order set, ensuring timely referrals. Ongoing evaluation will assess the effects on readmission rates, length of stay and hospice utilization in this targeted population, with initial trends showing positive results.
One important lesson learned was to successfully adopt a culture of earlier consults, the first team we need to educate, and influence was ourselves. Because our teams had primarily been utilized for acute, crisis-based palliative care, we were also our own barrier to early palliative care. We learned that tailoring triage workflows, aligning daily operations, and improving efficiency were important. Providing ongoing education and feedback to referring providers - highlighting the value of earlier palliative care - led to further utilization. Strong leadership support at all levels, including understanding of integrated economic value in our Integrated Delivery Network (IDN), was crucial to driving our project forward.
Authors
- Ying Li, MD, FAAHPM (Sentara Health)
- Kimberly St. Jean, MD (Sentara Health)