Community Health Workers: Enhancing Palliative Care for Underserved Populations
This study explores how community health workers (CHWs) impact palliative and hospice care access for marginalized patients. As non-clinical team members, CHWs bridge the gap between patients and providers, coordinate resources, and educate patients and families on the benefits of palliative and hospice services. In this quality improvement project, we observe how CHWs improve health outcomes by addressing social determinants of health (SDOH) and promoting palliation for patients diagnosed with chronic or terminal illnesses in underserved communities.
Palliative care-trained CHWs conducted home visits to facilitate patient-family centered conversations. Chart audits were completed on visits from August 2024 to March 2025. Two palliative care nurse practitioners reviewed the notes to assess benefits provided and barriers addressed. The review included two CHWs serving low-income communities in Chicago and one CHW serving vulnerable populations in Philadelphia.
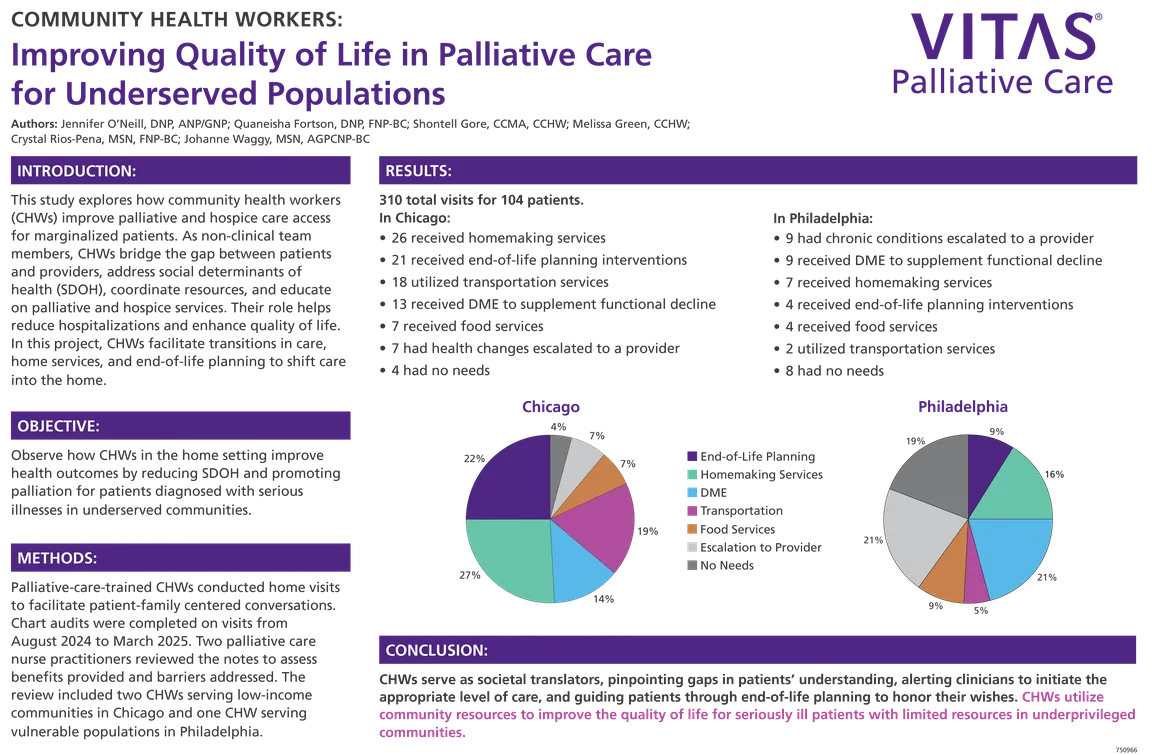
A total of 310 visits were completed for 104 patients. In Chicago, 21 patients received end of life planning, resulting in either a hospice admission or identification of a power of attorney and code status. 26 patients received homemaking services and 13 received durable medical equipment (DME) to supplement functional decline. 18 utilized transportation services to maintain continuity of care. 7 received food services and 7 had health changes escalated to a provider, while 4 had no identified needs.
In Philadelphia, 2 patients received transportation services, 9 received DME, and 7 were given homemakers. 4 patients received food services, 4 engaged in end-of-life planning interventions, 9 had chronic conditions escalated to a provider, and 8 had no identified needs.
Integrating CHWs into palliative care teams can greatly benefit patients and the healthcare system at large. CHWs serve as societal translators pinpointing gaps in patient understanding, alerting clinicians to initiate the appropriate level of care, and guiding patients through end-of-life planning to honor their wishes. Their role helps reduce costly and burdensome hospitalizations and facilitates utilization of community resources to improve the quality of life for patients with limited resources in underserved communities.
Authors
- Quaneisha Fortson, DNP, FNP-BC (Vitas Healthcare)
- Crystal Rios-Pena, MSN, FNP-BC (Vitas Healthcare)
- Johanne Waggy, MSN, AGPCNP-BS (Vitas Healthcare)
- Melissa Green, CCHW (Vitas Healthcare)
- Shontell Gore, CCMA, CCHW (Vitas Healthcare)
- Jennifer O'Neill, DNP, ANP/GNP (Vitas Healthcare)