Breaking the Glass Ceiling: Working to the Top of the Palliative Registered Nurse (RN) License
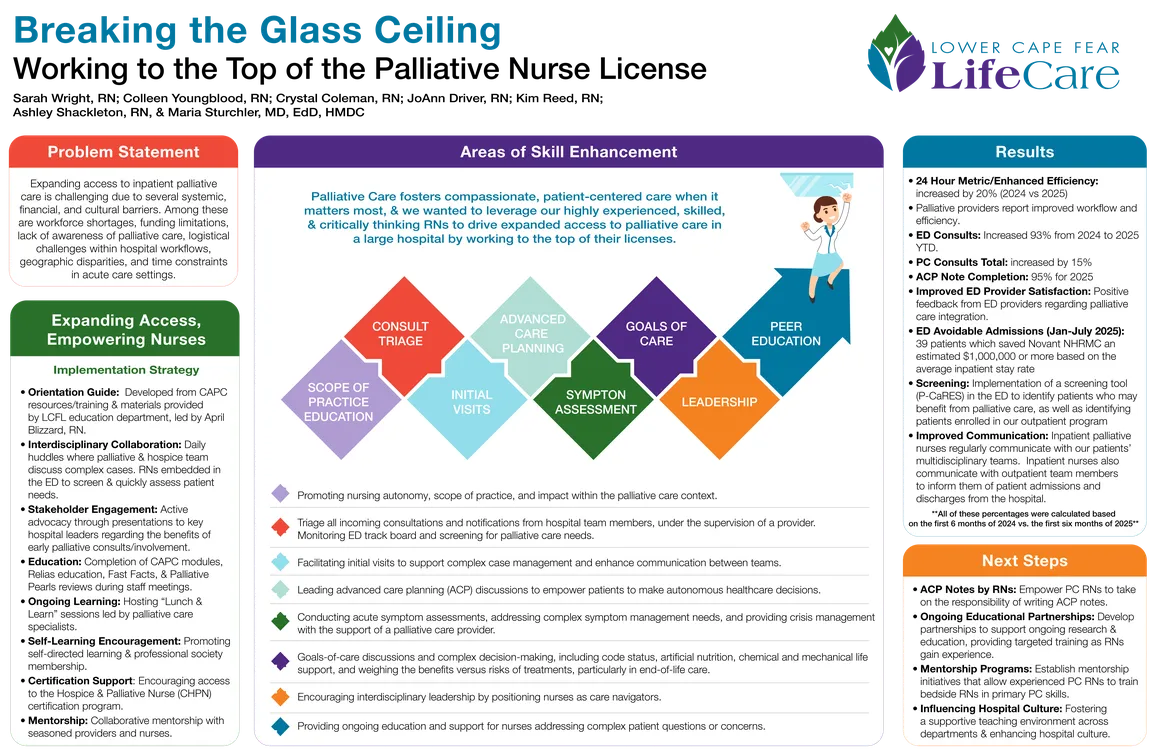
Palliative care (PC) is essential for addressing the complex needs of patients with serious illnesses, by ensuring comfort, dignity, and appropriate care. Many patients in the hospital setting face life-limiting conditions, acute symptom crises, or critical end-of-life decisions. However, expanding access to PC is challenging due to systemic, financial, and cultural barriers. Among these issues are workforce shortages, funding limitations, lack of awareness of palliative care, workflow challenges, geographic disparities, and time constraints in acute care settings. Because PC fosters compassionate, patient-centered care when it matters most, the team sought to drive expanded access to PC in a large hospital by empowering highly experienced, skilled, and critically thinking registered nurses (RNs) to practice at the top of their licenses.
Strategies included enabling RNs to advance their clinical practice by conducting symptom assessments and guiding advance care planning discussions, empowering autonomous clinical decision-making, promoting interdisciplinary leadership by positioning RNs as care navigators, and supporting complex case management to bridge communication between teams. The team piloted system integration by embedding PC RNs within key hospital units, such as the ED, to proactively identify and manage patients. We utilized our RNs' expertise to advocate for workflow changes, improved care protocols, and institutional commitment to expanding PC services through policy advocacy and educational initiatives. By elevating their clinical and leadership roles, RNs have been key to driving meaningful hospital-wide expansion of PC services.
We noted a significant increase in palliative consults, provider engagement, and satisfaction in the ED. Additionally, we have seen improved efficiency in inpatient PC consults, through leveraging our nurses to practice at the top of their licenses. Measuring whether palliative care nurses are practicing at the top of their license involves assessing their scope of practice, autonomy, and clinical impact. Key metrics included:
- Meeting the goal of addressing PC consults within 24 hours or less,
- Volume of ED-PC consults and trend thereof,
- Patient outcomes such as ACP completion, and
- Our RN team’s efficiency and role optimization.
These indicators demonstrate that our team’s nurses are utilized effectively to maximize team efficiency and have made our program highly agile in serving our patients.
Key lessons for programs aiming to expand access to PC in their care setting by leveraging their nursing talent include the importance of securing early leadership buy-in to ensure institutional support, resource allocation, and fostering robust interdisciplinary collaboration. Establishing educational partnerships is also essential to provide ongoing education that supports the professional growth of PC RNs over time. Finally, mentorship initiatives to allow adept PC RNs to train bedside nurses in primary PC skills - with experienced RNs teaching and supporting staff across departments - is a way to enhance patient care, hospital culture and morale. This approach can also motivate providers and departments that might be low utilizers of PC services to engage their patients with the benefits of PC.
Authors
- Colleen Youngblood, RN (Lower Cape Fear LifeCare – Wilmington)
- Crystal Coleman, RN (Lower Cape Fear LifeCare – Wilmington)
- JoAnn Driver, RN (Lower Cape Fear LifeCare – Wilmington)
- Kim Reed, RN, BSN (Lower Cape Fear LifeCare – Wilmington)
- Sarah Wright, RN, BSN (Lower Cape Fear LifeCare – Wilmington)
- Ashley Shackleton, RN, BSN (Lower Cape Fear LifeCare – Wilmington)
- Maria Sturchler, MD, EdD, HMDC (Lower Cape Fear LifeCare – Wilmington)