Course 1 of 6
Explore leadership frameworks, reflect on personal strengths, and identify opportunities for growth to become a more effective, high-impact leader.
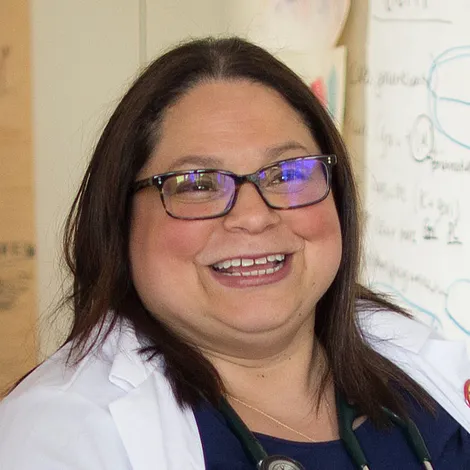
Dr. Fernandez is a palliative care physician and geriatrician. As Vice Chair of Education, Dr. Fernandez leads the largest geriatrics and palliative training programs in the country which trains 20% of the workforce and has served as a mentor to many students, residents, fellows and faculty. She has presented on many national and international meetings including the World Gerontology Conference, Society of General Internal Medicine, ACP Annual Meeting, AAHPM, AGS, the ACP International Meeting and the International Association for Medical Education Annual Conference. In 2011, she co-created the first integrated geriatrics and palliative care fellowship which has now been disseminated to 13 other institutions. She has received several teaching awards including the Leo Tow Gold Humanism Award, The Jeffrey T. Laitman, PhD Alumni Achievement Award at Icahn School of Medicine at Mount Sinai and Jacobi Medallion Award. In 2023, Dr. Fernandez became the principal investigator for the Brookdale Foundation Grant to further advance leadership training in geriatrics and palliative medicine and transform healthcare for older adults and those living with serious and chronic illness.
Course 1 of 6
Explore leadership frameworks, reflect on personal strengths, and identify opportunities for growth to become a more effective, high-impact leader.
Course 2 of 6
Learn practical communication skills—from active listening to managing difficult conversations—that build trust, strengthen teams, and enhance leadership impact.
Course 3 of 6
Explore how emotionally intelligent leadership builds trust, psychological safety, and collaboration to create high-performing health care teams.
Course 4 of 6
Build resilience and grit as a leader, using positive intelligence to overcome challenges, foster growth, and strengthen team productivity.
Course 5 of 6
Learn how to design inclusive, efficient workplaces that empower teams to contribute their unique strengths.
Course 6 of 6
Equip yourself with strategies to cultivate mission-driven, resilient teams and foster a work culture where staff thrive
Course 1 of 6
Understand how Medicare, Medicaid, and private payers share responsibility for health care costs, and the financial impact on patients and families.
Course 2 of 6
Examine what Medicare does and doesn't cover, while exploring the rise of Medicare Advantage and its impact on patients and providers.
Course 3 of 6
Learn how Medicaid and VA benefits support vulnerable patients and families needing palliative care, and who qualifies for these programs.
Course 4 of 6
Explore how fee-for-service payment works, its impact on quality, and strategies to optimize both revenue and performance under this model.
Course 5 of 6
Learn how value-based payment models tie quality to cost, and explore strategies for balancing priorities when navigating both fee-for-service and value-based care.
Course 6 of 6
Examine the rise of for-profit health care, why investors are drawn to the field, and the impact of profit incentives on care delivery.
Course 1 of 6
Develop systems-thinking skills to assess situations, engage key stakeholders, and strategically prioritize resources for effective leadership.
Course 2 of 6
Learn to strategically plan service expansion by conducting discovery, testing data-driven ideas, and engaging key decision-makers to secure resources.
Course 3 of 6
Learn how to balance planning with flexibility to navigate unplanned changes and maintain team stability.
Course 4 of 6
Learn to optimize staffing, collaborate across teams, and use operational data to improve service delivery and impact.
Course 5 of 6
Gain strategies to expand palliative care across settings and populations through thoughtful planning, partnerships, and collaboration.
Course 6 of 6
Learn to use metrics strategically to build a compelling business case, demonstrate program value, and secure long-term support.