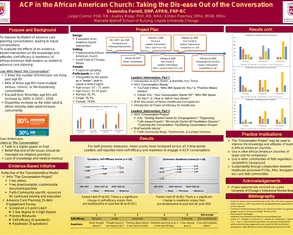
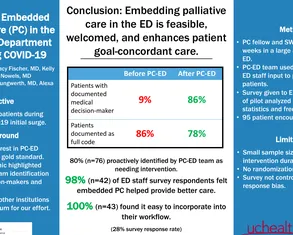
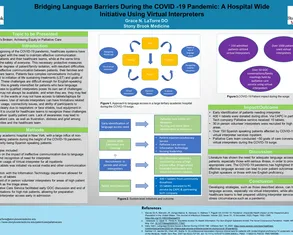
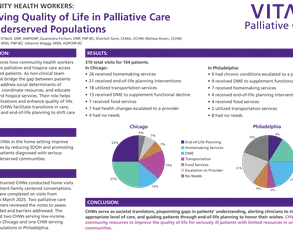
CAPC National Seminar and CAPC 2x4 Posters
View posters from the CAPC National Seminar (2019, 2025) and CAPC 2X4 (2020) events. The posters demonstrate how innovative palliative care programs all over the country are improving care quality for patients with serious illness. Connect to presenters via email to learn more and collaborate.